April Informed Newsletter 2023
April 19, 2023Grateful as Spring Blooms
As springtime blooms in our communities, we’re feeling grateful. Grateful for the warming temperatures and pleasant weather. For our members and the trust they place in us to be at their side. And for you – our hardworking, compassionate and exceptional provider partners, who take such great care of our members and so many others. Thank you for all that you do, every single day. We wish you a beautiful and blossoming springtime, as we commit to always being the partner you can count on.
***
Help us move the needle.
Together we can help people live their healthiest lives. Find reminders, tips and more in this section, to guide improvements in patient outcomes. Help us move the needle.
Quick Checklist: Support your patients with high blood pressure.
The Million Hearts® initiative of the U.S. Department of Health and Human Services wants to help you help your patients. Use this short checklist as a guide when your patients with high blood pressure come in to see you.
- Explain how you – and the other members of the patient’s care team – can help them control their blood pressure. Describe everyone’s roles.
- Review their blood pressure goal against their current readings.
- At the start of the visit, ask them: “What’s most important thing you want to accomplish during our visit today?” Their answer will help you set the agenda.
- Have an open conversation about their goals, achievements or setbacks, level of confidence, and any barriers or concerns. Ask how they’ve been feeling and doing since their last visit.
- Based on this conversation, help them set small, achievable goals. For example, if they’re trying to eat better, create goals for swapping out certain foods with low-sodium alternatives or for committing to a certain number of heart-healthy homecooked meals a week.
- For each goal you set, use the “Ask-Tell-Ask” technique:
- Ask permission to give them information about a certain topic. For example, if you want to create a goal for medication adherence, you could ask: “I’d like to tell you a few key things about your medications – is that OK?”
- Tell them what they need to know, once they’ve given you permission. Use simple words, pictures and diagrams to help them understand.
- Ask them to repeat the information back to you in their own words. This ensures they understood what you’ve taught them.
- To help them meet their goals, give the patient:
- A blood pressure tracker/log/journal with their specific target numbers written prominently.
- Instructions on how to take their blood pressure measurements at home – you can even give them the link to this helpful video.
- Heart-healthy diet and nutrition information.
- Exercise options and tips that are right for them.
- A list of support groups – and other resources – in the community.
- Remind them to measure and record their blood pressure readings at home on a regular basis – and to share these with you by phone, email or fax, and also during their next in-person visit.
A Tool for Identifying Preschool Children at Risk of Asthma
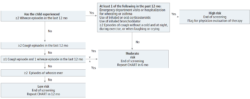
In a recent article in JAMA Network OpenTM (see citation below), researchers studied whether a symptom-based screening tool called CHART (CHILDhood Asthma Risk Tool) could improve doctors’ ability to identify preschool-aged children at risk of persistent asthma symptoms.
Their findings were encouraging. CHART was able to identify children at high risk of asthma at as early as 3 years of age – without the need for time-consuming and invasive tests. The researchers therefore believe that CHART can be easily used by doctors as a regular screening tool in primary care to help identify young children who might need monitoring, timely symptom control and/or the introduction of preventive therapies.
Here is the CHILDhood Asthma Risk Tool (CHART), from the article:
References Used for This Article
Myrtha E. Reyna, Ruixue Dai, Maxwell M. Tran, et al., “Development of a Symptom-Based Tool for Screening of Children at High Risk of Preschool Asthma,” JAMA Network Open, 2022;5(10):e2234714. doi:10.1001/jamanetworkopen.2022.34714. Click here for full article.
Preparing for the Next School Year with Yearly Wellness Checkups
As you know, you and your staff play a very large role in the health and well-being of your young patients. One way you do this is by having key conversations about their health, with both them and their parents or guardians. As you’re holding these conversations, make sure to remind parents and guardians how important it is to schedule their child’s yearly wellness checkup. Tell them how vital these are to detecting any health concerns in the early, more-treatable stages.
These wellness checkups are also key opportunities to make sure children are ready for the new school year. It’s important to discuss topics like:
- Eating well and nutrition.
- Physical activity levels and body mass index (BMI).
- Medications that may need updating.
This is also a great time to check the immunization status of your young patients. Here’s an immunization schedule from the CDC for reference, to help you guide the discussion with your patients and their parents/guardians. Some school districts require certain vaccinations for children entering specific grade levels, and depending on the age of your patient, they may be eligible for vaccines like Gardasil® (the HPV vaccine).
With summer fast approaching, the new school year will be starting before we know it. Reminding your young patients and their parents/guardians to schedule a wellness checkup at the end of this school year is a great way to be extra prepared before the busy summer season. Thank you for helping your young patients and their families think ahead and decrease the chances of appointment delays. We’re so grateful for all you do.
Chlamydia Screening Guidelines
As a helpful resource, here are the chlamydia screening recommendations and guidelines from the CDC.
Women
- Sexually active women under 25 years old should be screened.
- Sexually active women 25 and older should be screened if at higher risk (for example, due to having a new sex partner, more than one partner, a partner with concurrent partners or a partner with an STI).
- After treatment for chlamydia, women should retest three months later.
- Rectal chlamydial testing can be considered based on sexual behaviors and exposure, through shared decision-making with the patient.
Pregnant Women
- All pregnant women under 25 years old should be screened.
- Pregnant women 25 and older should be screened if at higher risk (for example, due to having a new sex partner, more than one partner, a partner with concurrent partners or a partner with an STI).
- Women under 25 and those 25+ at higher risk should retest during the third trimester.
- Pregnant women infected with chlamydia should have a “test of cure” (repeat testing after their completion of therapy, to track whether chlamydia is eradicated) at four weeks after their therapy is completed, and they should be retested within three months.
Men Who Have Sex with Women
- There’s insufficient evidence to recommend screening for heterosexual men who are at low risk for infection. However, screening can be considered for young men in high-prevalence clinical settings like adolescent clinics, STI/sexual health clinics and correctional facilities.
Men Who Have Sex with Men
- Screening at the sites of contact (urethra, rectum) is recommended at least once a year for sexually active individuals, regardless of condom use.
- Screening is recommended every three to six months for individuals at increased risk. This includes those on PrEP, individuals with HIV, and those with multiple sex partners or whose partner has multiple partners.
Transgender and Gender-Diverse Individuals
- Screening recommendations should be adapted based on the individual’s anatomy. For example, the above-mentioned annual, routine screening recommendation for women under 25 (and those 25+ at higher risk) should be extended to transgender men and gender-diverse individuals with a cervix.
- Consider screening at the rectal site, based on reported exposure and sexual behaviors.
Individuals with HIV
- For individuals who are sexually active, screen during their first HIV evaluation and at least annually thereafter.
- More frequent screening may be needed based on individual risk behaviors and the local epidemiology.
Help improve medication adherence.
We know how frustrating it is – you prescribe a medication, only to learn that your patient doesn’t take it or isn’t taking it right. Fortunately, there are steps you can take to help improve medication adherence. Here’s what you need to know and what you can do, provided from the American Medical Association’s Ed HubTM and its Steps Forward® educational guides.
- Patients are considered “nonadherent” if they take less than 80% of their prescribed medication(s).
- Nonadherence is very common – about 50% of the time, patients don’t take their drugs as prescribed.
- It’s serious – nonadherence can lead to unnecessary health complications, hospitalizations and emergency department visits.
- Patients are often embarrassed to tell their doctor that they’re not taking their medications as prescribed.
- Common reasons for nonadherence include: the cost of drugs; a lack of understanding regarding how to correctly take them – or even why they’re important or how they help them; drug scarcity; time constraints, lack of transportation and other access difficulties; mistrust of the medical system; and simple forgetfulness.
- To help improve your patients’ adherence:
- When evaluating your patients, be aware that nonadherence may be a reason why their condition isn’t under control.
- Regularly ask your patients about medication adherence. Make this part of your routine process during visits.
- Create a friendly, welcoming environment free of shame and blame. Patients will find it easier to talk openly and honestly.
- In talking with your patients, identify the specific reason(s) why they’re not taking their medicines (or not taking them correctly).
- Create an adherence plan that’s specifically catered to each patient’s unique reason(s) for nonadherence. And set them up for success – give them the information, resources and assistance that can help them overcome their specific barriers.
- Let your patients be involved in creating their adherence plans – this gives them a sense of ownership and greater motivation.
With you at their side, your patients can start taking their medications correctly, consistently and with improved optimism. Thank you for being such a key partner in their lives.
Nutritional Recommendations for Patients with Congestive Heart Failure
As you know, proper nutrition is very important for patients with congestive heart failure (CHF). Here are some of the latest recommendations, from the Physicians Committee for Responsible Medicine’s Nutrition Guide for Clinicians.
- In the past, the main focus for people with CHF was lowering their sodium intake. This is still important, but recent findings suggest other areas of focus as well.
- Limiting extra sodium helps lower the risk for CHF – but the degree of sodium restriction has been greatly debated. Most evidence supports a moderate level of sodium restriction to 2,000 – 3,000 mg per day.
- Macronutrient nutrition may impact prevention more than previously thought.
- Avoiding saturated fat and fried food is also now seen as key.
- High amounts of red meats, eggs and fried foods can increase the risk of CHF. These are all sources of advanced glycation products, which have been linked to the severity of heart failure and are independent predictors for cardiac issues.
- Diets that are higher in fruits, vegetables, fish and unsaturated fat, and lower in meat, can help lower the risk for CHF.
- Patients can aim for a minimum of five (combined) fruit and vegetable servings each day. Vegetables appear to be the most beneficial.
- Plant-based diets have also been shown to lower risk factors.
- Certain dietary supplements (thiamine, coenzyme Q10) can also help.
- Consider thiamine supplements for patients treated with diuretics. See the guide for more specifics.
- Monitor your patients’ magnesium status. See the guide for more specifics.
Heart failure is usually progressive – but you may be able to help your patients improve their heart health, ease their symptoms and prolong their survival by having them follow the nutritional recommendations above, take their medications as prescribed and restrict their fluids. Exercise conditioning and family support are also key. Thank you for all your help for these patients and their needs.
HEDIS Quality Measure – Plan All-Cause Readmissions (PCR)
By working together, we can keep patients from unnecessary return trips to the hospital. The Healthcare Effectiveness Data and Information Set (HEDIS®) is a set of standards that helps us together assess the care patients receive. This article gives you information on the HEDIS quality measure for preventing readmissions, and tips on how to meet this measure and provide best care.
Why’s this measure important?
Keeping patients out of the hospital can greatly improve their health. A “readmission,” by definition, occurs when a patient is discharged from the hospital but then admitted back in within a short period of time. Unplanned readmissions are linked to higher mortality and increased healthcare costs. High rates of readmission may point to inadequate care (by providers) or a lack of appropriate post-discharge planning, follow up and care coordination (by the health plan and providers).
What’s the HEDIS measure?
HEDIS looks at, and reports, the following:
- The number of acute inpatient and observation hospital/facility stays that were followed, within 30 days of discharge, by an unplanned acute hospital/facility readmission (for any diagnosis). It measures this for patients 18 years old and above. The number is measured as a rate – a lower rate means a better score.
Notes: An acute discharge can be from any type of facility, including behavioral health facilities. And the measure is based on discharges – not patients specifically – so multiple admissions are counted more than once. - In addition to the observed numbers, health plans also need to report a predicted probability of acute hospital/facility readmission.
Tips and Best Practices to Help Lower Readmissions
- Providers should create – and put into place – a “safe discharge plan” that includes, among other things:
- Easy-to-understand post-discharge instructions for the patient and their loved ones.
- Medication reconciliation that clearly notes the patient’s discharge medications and those they were taking prior to admission.
- A process for making sure patients understand how to take their medications. It’s also key to let them know what each medicine does and how it helps them.
- A process for engaging patients, their loved ones, and their other doctors and healthcare specialists in coordinated care.
- Detailed plans for smooth transitional care and, if relevant, the implementation of a robust home healthcare program with oversight and follow up.
- Scheduling of a seven-day follow-up appointment.
- A post-discharge phone call within a specified time frame to check on the patient’s condition and needs, and to answer any questions they may have.
- At the patient’s seven-day follow-up appointment, you should:
- Thoroughly review their instructions given at discharge.
- Review their medications, medication changes and instructions on how to take each drug.
- Make sure they did – or will soon – fill their prescriptions.
- Schedule their next follow-up appointment.
Information in this article is based on National Committee for Quality Assurance (NCQA) HEDIS® technical specifications. For details, visit ncqa.org.
***
Coding Counts:
Documenting, Reporting and Coding Drug Dependence
Supporting documentation and accurate coding are key to making sure your patients receive the care they need. For patients with drug dependency, screening, prevention and coordination of care help provide opportunities for early intervention and improved outcomes. Here are some key tips for documenting, reporting and coding drug dependence.
Be specific.
Per ICD-10-CM guidelines, coding for drug dependence is based on provider documentation, making it key to distinguish dependence from use and abuse.
Drug dependence is defined as a chronic mental and physical state where the patient needs to use a substance to function normally and can experience signs of withdrawal upon cessation of the substance. Signs and symptoms indicating drug dependence may include:
- Increased tolerance.
- Physical withdrawal symptoms.
- Time and effort to get, use and recover from effects.
- Withdrawal from social activities.
- Continued use despite physical, psychological and family/social problems caused by ongoing drug use.
Medical Conditions Due to Drug Dependence
ICD-10-CM includes codes for disorders related to drug dependence and these should be reported when complications associated with the drug dependence are documented. Complications can include:
| · Amnestic disorder. | · Intoxication. |
| · Anxiety disorder. | · Mood disorder. |
| · Delirium. | · Perceptual disturbance. |
| · Delusions. | · Psychotic disorder. |
| · Dementia. | · Sexual dysfunction. |
| · Flashbacks. | · Sleep disorder. |
| · Hallucinations. | · Withdrawal. |
History Of = In Remission
In ICD-10-CM, history of drug dependence is reported as “drug dependence, in remission” to indicate that the clinical criteria for drug dependence is no longer met.
What to Report When Use, Abuse and Dependence Are Documented
- If both abuse and dependence are documented, assign only the code for dependence.
- If both use and dependence are documented, assign only the code for dependence.
- If use, abuse and dependence are all documented, assign only the code for dependence.
We thank you for your exceptional professionalism and attention to detail, and we’re here to help. To find more coding resources, visit our Coding Counts page. Thank you for your continued care and dedication to our members’ health.
Questions?
Please contact us at CodingCounts@HealthAlliance.org.
References Used for This Article
ICD-10-CM Official Guidelines for Coding and Reporting
Optum EncoderPro
Johns Hopkins Medicine, HopkinsMedicine.org
Help us transform diabetes care delivery with Virta.
We’re excited to now offer Virta Health to our members with diabetes who are on our fully insured health plans. Among the services offered by Virta is type 2 diabetes reversal, which includes support from a provider-based care team, nutritional therapy and coaching, and mobile app-based resources. This protocol lowers blood sugar and A1C, supports weight loss, and reduces or eliminates the need for diabetic medications for some patients. Your patients can call the number on the back of their health plan member ID card to see if their plan includes Virta.
How does Virta work?
Virta includes type 2 diabetes reversal services. Once a patient’s enrolled in Virta, they work with a health coach and receive a welcome kit that includes a connected scale, a glucose and ketone monitor, testing supplies, and literature on the Virta treatment. Patients log their biomarkers regularly and begin making dietary changes under guidance from their Virta care team, which includes their health coach and a provider.
There’s no out-of-pocket cost for these members to participate in any Virta service. All costs are submitted to us through medical claims. To learn more about the Virta patient experience, visit: www.virtahealth.com/join/hally.
With Virta, your patients could see:
- Diabetes Reversal – 60% of patients achieved subdiabetic A1C and elimination of all diabetes-specific medications after one year.1
- Rx Elimination – 59% average diabetes Rx cost reduction at one year, based on peer-reviewed clinical data.1
- Cost Savings – $503 per-patient-per-month cost savings over two years, based on claims analysis using real-world data.2
Want to learn more? Contact your provider relations specialist for more details.
References Used for This Article
- SJ Hallberg, et al., Diabetes Therapy, 2018;9(2):583-612. For patients completing 1 year of treatment.
- Virta Health, “Analysis of Type 2 Diabetes Reversal Cost Savings,” Sept. 2021.
New Low-Cost Option for
Patients with Autoimmune Disorders
Note: This article does not apply to Medicare plans.
Note: This article does not apply to Reid Health Alliance Medicare branded plans.
We have good news for your patients with autoimmune disorders – a new adalimumab biosimilar product, Amjevita, has been added to our formulary. The manufacturer has priced Amjevita at two levels based on the National Drug Code (NDC). We’ve chosen to add only the lower-cost NDCs to Commercial formularies with prior authorization, in parity with Humira. Humira will continue to be available on our formulary. Please be aware of this new formulary alternative and the potential for savings for your patients struggling with drug costs.
Updates to High Cost Medical Drugs List
See the table below for changes to the High Cost Medical Drugs List with effective dates.
Note: Medications removed from the High Cost Medical Drugs List may still require prior authorization.
Note: This article/table does not apply to Medicare plans.
Note: This article/table does not apply to Reid Health Alliance Medicare branded plans.
| Drug Therapy | Drug Name | Code | PA | Effective | Preferred
Vendor |
Contact
Number |
Change |
| Oncology – Injectable | IMJUDO | MSC | YES | 2/1/2023 | Optum Specialty | (855) 427-4682 | Added |
Midwest – Pharmacy Updates
All Plans
Oncology/Hematology
Formulary Additions
- Enjaymo (sutimlimab-jome)—Used to decrease the need for red blood cell transfusion due to hemolysis in adults with cold agglutinin disease
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Pyrukynd (mitapivat)—Treatment of hemolytic anemia in adults with pyruvate kinase deficiency
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Vijoice (alpelisib)—Treatment of severe manifestations of PIK3CA-related overgrowth spectrum in patients ≥2 years of age who require systemic therapy
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Hemgenix (etranacogene dezaparvovec)—Treatment of hemophilia B (congenital factor IX deficiency) in adults who currently use factor IX prophylaxis therapy, or have current or historical life-threatening hemorrhage, or have repeated, serious spontaneous bleeding episodes
- Formulary placement recommendations
- Commercial— Tier 6, Non-Preferred/Non-Formulary Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Zynteglo (betibeglogene autotemcel)—Treatment of beta thalassemia in adult and pediatric patients who require regular red blood cell transfusions
- Formulary placement recommendations
- Commercial—Not Covered
- Medicare—Not Covered
- Formulary placement recommendations
| New Oncology Drug | Indication | Coverage Recommendation |
| Adstiladrin (nadofaragene firadenovec-vncg); gene therapy | Bladder cancer: Treatment of adult patients with high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Carvykti (ciltacabtagene autoleucel); CAR-T 100000000 cells | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults after ≥4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Elahere (mirvetuximab soravtansine); 100 MG/20ML IV solution | Epithelial ovarian, fallopian tube, or primary peritoneal cancer, folate receptor-alpha positive, platinum-resistant: Treatment of folate receptor-alpha positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer in adults, who have received 1 to 3 prior systemic treatment regimens. Select patients for therapy based on an FDA-approved test. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Imjudo (tremelimumab); 300 mg/15 mL and 25 mg/1.25 mL IV solution | Hepatocellular carcinoma, unresectable: Treatment of unresectable hepatocellular carcinoma (in combination with durvalumab) in adults. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Kimmtrak (tebentafusp); 100 mcg/0.5 mL IV solution | Uveal melanoma, unresectable or metastatic: Treatment of HLA-A*02:01-positive unresectable or metastatic uveal melanoma in adults. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Krazati (adagrasib); 200mg oral tablet | Non–small cell lung cancer, locally advanced or metastatic, KRAS G12C-mutated: Treatment of KRAS G12C-mutated locally advanced or metastatic non–small cell lung cancer (NSCLC), as determined by an approved test, in adults who have received at least 1 prior systemic therapy. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Lunsumio (mosunetuzumab-axgb); 1mg/mL IV solution | Follicular Lymphoma: Treatment of adult patients with relapsed or refractory (R/R) follicular lymphoma (FL) after two or more lines of systemic therapy | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Lytgobi (futibatinib); 4mg oral tablet | Cholangiocarcinoma, intrahepatic, previously treated, unresectable locally advanced or metastatic: Treatment of previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma harboring fibroblast growth factor receptor 2 gene fusions or other rearrangements in adults. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Opdualag (nivolumab/ relatlimab); 240mg/80mg per 20mL IV solution | Melanoma, unresectable or metastatic: Treatment of unresectable or metastatic melanoma in adult and pediatric patients ≥12 years of age. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Rezlidhia (olutasidenib); 150mg oral capsule | Acute myeloid leukemia, relapsed or refractory: Treatment of relapsed or refractory acute myeloid leukemia in adults with a susceptible isocitrate dehydrogenase-1 mutation as detected by an FDA-approved test. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Tecvayli (teclistamab); 10 mg/mL and 90 mg/mL IV solution | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults who have received at least 4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Vonjo (pacritinib); 200mg oral capsule | Myelofibrosis: Treatment of intermediate or high-risk primary or secondary (postpolycythemia vera or postessential thrombocythemia) myelofibrosis in adults with a platelet count <50,000/mm3 | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Xalkori (crizotinib); 200mg and 250mg oral tablet | Inflammatory myofibroblastic tumor, ALK-positive, unresectable, recurrent, or refractory: Treatment of ALK-positive unresectable, recurrent, or refractory inflammatory myofibroblastic tumor in adult and pediatric patients ≥1 year of age. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
New Oncology Indications (could be Part B or D, depending on member)
| Drug | New Indication | Coverage |
| Brukinsa (zanubrutinib) | Lymphocytic lymphoma: treatment of adult patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Enhertu (fam-trastuzumab deruxtecan) | Breast cancer, unresectable or metastatic, HER2-low: Treatment of unresectable or metastatic HER2-low (immunohistochemical [IHC] 1+ or IHC 2+ and negative in situ hybridization [ISH-]) breast cancer (as determined by an approved test) in adults who have received a prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant therapy. | Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Ibrance (palbociclib) | Breast cancer, advanced (with disease progression following endocrine therapy): Treatment of HR-positive, HER2-negative advanced or metastatic breast cancer (in combination with fulvestrant) in adult patients with disease progression following endocrine therapy. | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Libtayo (cemiplimab) | Non–small cell lung cancer, locally advanced or metastatic:
First-line treatment (single-agent or in combination) of non–small cell lung cancer in adults whose tumors have high PD-L1 expression (Tumor Proportion Score ≥50%) as determined by an approved test, with no EGFR, ALK, or ROS1 aberrations, and with locally advanced (in patients who are not candidates for surgical resection or definitive chemoradiation) or metastatic disease. |
Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Nubeqa (darolutamide) | Prostate cancer, metastatic, hormone-sensitive: Treatment of metastatic hormone-sensitive prostate cancer (in combination with docetaxel) in adults. | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Tecentriq (atezolizumab) | Alveolar soft part sarcoma: treatment of adult and pediatric patients 2 years of age and older with unresectable or metastatic alveolar soft part sarcoma (ASPS). | Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Tukysa (tucatinib) | Colorectal cancer: treatment of adult patients with RAS wild-type, human epidermal growth factor receptor 2 (HER2)-positive unresectable or metastatic colorectal cancer that has progressed following treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy in combination with trastuzumab | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Xeloda (capecitabine) | Pancreatic adenocarcinoma: Adjuvant treatment of adults with pancreatic adenocarcinoma as a component of a combination chemotherapy regimen
Gastroesophageal junction adenocarcinoma: Treatment of adults with HER2-overexpressing metastatic gastric or gastroesophageal junction adenocarcinoma who have not received prior treatment for metastatic disease as a component of a combination regimen AND Treatment of adults with unresectable or metastatic gastric, esophageal, or gastroesophageal junction cancer as a component of a combination chemotherapy regimen |
Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part B |
Infectious Disease
Formulary Additions
- Vivjoa (oteseconazole)—To reduce the incidence of recurrent vulvovaginal candidiasis (RVVC) in females with a history of RVVC who are not of reproductive potential, alone or in combination with fluconazole
- Formulary placement recommendations
- Commercial—Non-Preferred Brand with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Rebyota (fecal microbiota, live-jslm)—For the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Sunlenca (lenacapavir)—Treatment of HIV-1 infection, in combination with other antiretrovirals, in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy (oral tablet) or Medical (injectable)
- Medicare—Tier 5 Pharmacy Specialty
- Formulary placement recommendations
Commercial
Oncology/Hematology
Criteria Changes*
- Jakafi—Added criteria for chronic graft versus host disease
- Oxbryta—Updated criteria language, specified drug in quantity limit
- Promacta—Added coverage criteria for hepatitis C related thrombocytopenia
- Soliris—Updated coverage criteria to include REMS program and review by medical director, exclusion criteria and HCPCS code
- Ultomiris—Added criteria for Myasthenia Gravis, updated exclusion criteria
- Tavalisse—Added specialist and age criteria
Infectious Disease
Criteria Changes*
- Brexafemme (ibrexafungerp)—Added criteria for new indication RVVC, exclusion criteria
- Hepatitis B Treatment – Hepsera, Baraclude, Vemlidy & Pegasys—Added Pegasys to the policy, updated age criteria
- Pretomanid—Updated diagnosis and exclusion criteria
- Preventive Vaccine Policy—Added criteria for Dengvaxia, updated policy purpose and statement
- Sirturo (bedaquiline)—Added specialist and age criteria
Miscellaneous Criteria Changes*
- Diabetes Drug Therapies—Updated GLP-1/Mounjaro criteria, removed Adlyxin (discontinued)
- Rituxan, Ruxience, and Truxima (rituximab)—Added criteria for cold agglutinin disease
- Weight Loss Medications—Added approval period language
- NOTE: Only select Self-Funded plans currently cover weight loss medications.
- Non-Radiographical Axial Sponyloarthritis—Created policy that defines the criteria for coverage of immunomodulators used in the treatment of Non-radiographic Axial Spondyloarthritis (nr-axSpA) (currently Cimzia, Rinvoq Taltz, and Cosentyx under the Specialty Pharmacy benefit)
Commercial Tier Changes
Positive Changes
- Diazepam oral tablets and solution: Move from Non-Preferred Generic to Preferred Generic
- Brand Valium oral tablets: Move from Non-Preferred Brand to Preferred Brand
- Feedback from the market conduct exam requires alcohol withdrawal products be covered at Preferred status
Note: There were no negative changes.
* Members currently utilizing these therapies will not experience a disruption.
Please Note: The P&T Committee meets bimonthly, and formulary changes and criteria changes can occur during the meetings. Negative formulary changes are made effective on 1/1 and 7/1, while positive formulary changes are effective immediately to better serve our members and providers. Drug coverage and policies in the following categories will be reviewed during the remainder of 2023 and changes may be made:
- April Meeting: Rheumatology, Gastroenterology, Dermatology.
- June Meeting: Cardiology, Endocrinology, Pulmonology.
- August Meeting: Neurology, Psychiatry, Pain.
- October Meeting: Ophthalmology, Urology, Rare Diseases.
- December Meeting: Specialty and Medicare.
Northwest – Pharmacy Updates
All Plans
Oncology/Hematology
Formulary Additions
- Enjaymo (sutimlimab-jome)—Used to decrease the need for red blood cell transfusion due to hemolysis in adults with cold agglutinin disease
- Formulary placement recommendations
- WA Individual—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Pyrukynd (mitapivat)—Treatment of hemolytic anemia in adults with pyruvate kinase deficiency
- Formulary placement recommendations
- WA Individual—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Vijoice (alpelisib)—Treatment of severe manifestations of PIK3CA-related overgrowth spectrum in patients ≥2 years of age who require systemic therapy
- Formulary placement recommendations
- WA Individual—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Hemgenix (etranacogene dezaparvovec)—Treatment of hemophilia B (congenital factor IX deficiency) in adults who currently use factor IX prophylaxis therapy, or have current or historical life-threatening hemorrhage, or have repeated, serious spontaneous bleeding episodes
- Formulary placement recommendations
- WA Individual—Tier 6, Non-Preferred/Non-Formulary Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Zynteglo (betibeglogene autotemcel)—Treatment of beta thalassemia in adult and pediatric patients who require regular red blood cell transfusions
- Formulary placement recommendations
- WA Individual—Not Covered
- Medicare—Not Covered
- Formulary placement recommendations
| New Oncology Drug | Indication | Coverage Recommendation |
| Adstiladrin (nadofaragene firadenovec-vncg); gene therapy | Bladder cancer: Treatment of adult patients with high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Carvykti (ciltacabtagene autoleucel); CAR-T 100000000 cells | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults after ≥4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Elahere (mirvetuximab soravtansine); 100 MG/20ML IV solution | Epithelial ovarian, fallopian tube, or primary peritoneal cancer, folate receptor-alpha positive, platinum-resistant: Treatment of folate receptor-alpha positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer in adults, who have received 1 to 3 prior systemic treatment regimens. Select patients for therapy based on an FDA-approved test. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Imjudo (tremelimumab); 300 mg/15 mL and 25 mg/1.25 mL IV solution | Hepatocellular carcinoma, unresectable: Treatment of unresectable hepatocellular carcinoma (in combination with durvalumab) in adults. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Kimmtrak (tebentafusp); 100 mcg/0.5 mL IV solution | Uveal melanoma, unresectable or metastatic: Treatment of HLA-A*02:01-positive unresectable or metastatic uveal melanoma in adults. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Krazati (adagrasib); 200mg oral tablet | Non–small cell lung cancer, locally advanced or metastatic, KRAS G12C-mutated: Treatment of KRAS G12C-mutated locally advanced or metastatic non–small cell lung cancer (NSCLC), as determined by an approved test, in adults who have received at least 1 prior systemic therapy. | WA Individual: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Lunsumio (mosunetuzumab-axgb); 1mg/mL IV solution | Follicular Lymphoma: Treatment of adult patients with relapsed or refractory (R/R) follicular lymphoma (FL) after two or more lines of systemic therapy | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Lytgobi (futibatinib); 4mg oral tablet | Cholangiocarcinoma, intrahepatic, previously treated, unresectable locally advanced or metastatic: Treatment of previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma harboring fibroblast growth factor receptor 2 gene fusions or other rearrangements in adults. | WA Individual: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Opdualag (nivolumab/ relatlimab); 240mg/80mg per 20mL IV solution | Melanoma, unresectable or metastatic: Treatment of unresectable or metastatic melanoma in adult and pediatric patients ≥12 years of age. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Rezlidhia (olutasidenib); 150mg oral capsule | Acute myeloid leukemia, relapsed or refractory: Treatment of relapsed or refractory acute myeloid leukemia in adults with a susceptible isocitrate dehydrogenase-1 mutation as detected by an FDA-approved test. | WA Individual: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Tecvayli (teclistamab); 10 mg/mL and 90 mg/mL IV solution | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults who have received at least 4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | WA Individual: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Vonjo (pacritinib); 200mg oral capsule | Myelofibrosis: Treatment of intermediate or high-risk primary or secondary (postpolycythemia vera or postessential thrombocythemia) myelofibrosis in adults with a platelet count <50,000/mm3 | WA Individual: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Xalkori (crizotinib); 200mg and 250mg oral tablet | Inflammatory myofibroblastic tumor, ALK-positive, unresectable, recurrent, or refractory: Treatment of ALK-positive unresectable, recurrent, or refractory inflammatory myofibroblastic tumor in adult and pediatric patients ≥1 year of age. | WA Individual: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
New Oncology Indications (could be Part B or D, depending on member)
| Drug | New Indication | Coverage |
| Brukinsa (zanubrutinib) | Lymphocytic lymphoma: treatment of adult patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). | WA Individual: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Enhertu (fam-trastuzumab deruxtecan) | Breast cancer, unresectable or metastatic, HER2-low: Treatment of unresectable or metastatic HER2-low (immunohistochemical [IHC] 1+ or IHC 2+ and negative in situ hybridization [ISH-]) breast cancer (as determined by an approved test) in adults who have received a prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant therapy. | WA Individual: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Ibrance (palbociclib) | Breast cancer, advanced (with disease progression following endocrine therapy): Treatment of HR-positive, HER2-negative advanced or metastatic breast cancer (in combination with fulvestrant) in adult patients with disease progression following endocrine therapy. | WA Individual: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Libtayo (cemiplimab) | Non–small cell lung cancer, locally advanced or metastatic:
First-line treatment (single-agent or in combination) of non–small cell lung cancer in adults whose tumors have high PD-L1 expression (Tumor Proportion Score ≥50%) as determined by an approved test, with no EGFR, ALK, or ROS1 aberrations, and with locally advanced (in patients who are not candidates for surgical resection or definitive chemoradiation) or metastatic disease. |
WA Individual: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Nubeqa (darolutamide) | Prostate cancer, metastatic, hormone-sensitive: Treatment of metastatic hormone-sensitive prostate cancer (in combination with docetaxel) in adults. | WA Individual: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Tecentriq (atezolizumab) | Alveolar soft part sarcoma: treatment of adult and pediatric patients 2 years of age and older with unresectable or metastatic alveolar soft part sarcoma (ASPS). | WA Individual: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Tukysa (tucatinib) | Colorectal cancer: treatment of adult patients with RAS wild-type, human epidermal growth factor receptor 2 (HER2)-positive unresectable or metastatic colorectal cancer that has progressed following treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy in combination with trastuzumab | WA Individual: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Xeloda (capecitabine) | Pancreatic adenocarcinoma: Adjuvant treatment of adults with pancreatic adenocarcinoma as a component of a combination chemotherapy regimen
Gastroesophageal junction adenocarcinoma: Treatment of adults with HER2-overexpressing metastatic gastric or gastroesophageal junction adenocarcinoma who have not received prior treatment for metastatic disease as a component of a combination regimen AND Treatment of adults with unresectable or metastatic gastric, esophageal, or gastroesophageal junction cancer as a component of a combination chemotherapy regimen |
WA Individual: Non Preferred Specialty Pharmacy with PA
Medicare: Part B |
Infectious Disease
Formulary Additions
- Vivjoa (oteseconazole)—To reduce the incidence of recurrent vulvovaginal candidiasis (RVVC) in females with a history of RVVC who are not of reproductive potential, alone or in combination with fluconazole
- Formulary placement recommendations
- WA Individual—Non-Preferred Brand with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Rebyota (fecal microbiota, live-jslm)—For the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI
- Formulary placement recommendations
- WA Individual—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Sunlenca (lenacapavir)—Treatment of HIV-1 infection, in combination with other antiretrovirals, in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations
- Formulary placement recommendations
- WA Individual—Non-Preferred Specialty Pharmacy (oral tablet) or Medical (injectable)
- Medicare—Tier 5 Pharmacy Specialty
- Formulary placement recommendations
WA Individual
Oncology/Hematology
Criteria Changes*
- Jakafi—Added criteria for chronic graft versus host disease
- Oxbryta—Updated criteria language, specified drug in quantity limit
- Promacta—Added coverage criteria for hepatitis C related thrombocytopenia
- Soliris—Updated coverage criteria to include REMS program and review by medical director, exclusion criteria and HCPCS code
- Ultomiris—Added criteria for Myasthenia Gravis, updated exclusion criteria
- Tavalisse—Added specialist and age criteria
Infectious Disease
Criteria Changes*
- Brexafemme (ibrexafungerp)—Added criteria for new indication RVVC, exclusion criteria
- Hepatitis B Treatment – Hepsera, Baraclude, Vemlidy & Pegasys—Added Pegasys to the policy, updated age criteria
- Pretomanid—Updated diagnosis and exclusion criteria
- Preventive Vaccine Policy—Added criteria for Dengvaxia, updated policy purpose and statement
- Sirturo (bedaquiline)—Added specialist and age criteria
Miscellaneous Criteria Changes*
- Diabetes Drug Therapies—Updated GLP-1/Mounjaro criteria, removed Adlyxin (discontinued)
- Rituxan, Ruxience, and Truxima (rituximab)—Added criteria for cold agglutinin disease
- Weight Loss Medications—Added approval period language
- NOTE: Only select Self-Funded plans currently cover weight loss medications.
- Non-Radiographical Axial Sponyloarthritis—Created policy that defines the criteria for coverage of immunomodulators used in the treatment of Non-radiographic Axial Spondyloarthritis (nr-axSpA) (currently Cimzia, Rinvoq Taltz, and Cosentyx under the Specialty Pharmacy benefit)
WA Individual Tier Changes
Positive Changes
- Diazepam oral tablets and solution: Move from Non-Preferred Generic to Preferred Generic
- Brand Valium oral tablets: Move from Non-Preferred Brand to Preferred Brand
- Feedback from the market conduct exam requires alcohol withdrawal products be covered at Preferred status
Note: There were no negative changes.
* Members currently utilizing these therapies will not experience a disruption.
Please Note: The P&T Committee meets bimonthly, and formulary changes and criteria changes can occur during the meetings. Negative formulary changes are made effective on 1/1 and 7/1, while positive formulary changes are effective immediately to better serve our members and providers. Drug coverage and policies in the following categories will be reviewed during the remainder of 2023 and changes may be made:
- April Meeting: Rheumatology, Gastroenterology, Dermatology.
- June Meeting: Cardiology, Endocrinology, Pulmonology.
- August Meeting: Neurology, Psychiatry, Pain.
- October Meeting: Ophthalmology, Urology, Rare Diseases.
- December Meeting: Specialty and Medicare.
Carle – Pharmacy Updates
All Plans
Oncology/Hematology
Formulary Additions
- Enjaymo (sutimlimab-jome)—Used to decrease the need for red blood cell transfusion due to hemolysis in adults with cold agglutinin disease
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Pyrukynd (mitapivat)—Treatment of hemolytic anemia in adults with pyruvate kinase deficiency
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Vijoice (alpelisib)—Treatment of severe manifestations of PIK3CA-related overgrowth spectrum in patients ≥2 years of age who require systemic therapy
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Hemgenix (etranacogene dezaparvovec)—Treatment of hemophilia B (congenital factor IX deficiency) in adults who currently use factor IX prophylaxis therapy, or have current or historical life-threatening hemorrhage, or have repeated, serious spontaneous bleeding episodes
- Formulary placement recommendations
- Commercial— Tier 6, Non-Preferred/Non-Formulary Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Zynteglo (betibeglogene autotemcel)—Treatment of beta thalassemia in adult and pediatric patients who require regular red blood cell transfusions
- Formulary placement recommendations
- Commercial—Not Covered
- Medicare—Not Covered
- Formulary placement recommendations
| New Oncology Drug | Indication | Coverage Recommendation |
| Adstiladrin (nadofaragene firadenovec-vncg); gene therapy | Bladder cancer: Treatment of adult patients with high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Carvykti (ciltacabtagene autoleucel); CAR-T 100000000 cells | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults after ≥4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Elahere (mirvetuximab soravtansine); 100 MG/20ML IV solution | Epithelial ovarian, fallopian tube, or primary peritoneal cancer, folate receptor-alpha positive, platinum-resistant: Treatment of folate receptor-alpha positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer in adults, who have received 1 to 3 prior systemic treatment regimens. Select patients for therapy based on an FDA-approved test. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Imjudo (tremelimumab); 300 mg/15 mL and 25 mg/1.25 mL IV solution | Hepatocellular carcinoma, unresectable: Treatment of unresectable hepatocellular carcinoma (in combination with durvalumab) in adults. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Kimmtrak (tebentafusp); 100 mcg/0.5 mL IV solution | Uveal melanoma, unresectable or metastatic: Treatment of HLA-A*02:01-positive unresectable or metastatic uveal melanoma in adults. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Krazati (adagrasib); 200mg oral tablet | Non–small cell lung cancer, locally advanced or metastatic, KRAS G12C-mutated: Treatment of KRAS G12C-mutated locally advanced or metastatic non–small cell lung cancer (NSCLC), as determined by an approved test, in adults who have received at least 1 prior systemic therapy. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Lunsumio (mosunetuzumab-axgb); 1mg/mL IV solution | Follicular Lymphoma: Treatment of adult patients with relapsed or refractory (R/R) follicular lymphoma (FL) after two or more lines of systemic therapy | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Lytgobi (futibatinib); 4mg oral tablet | Cholangiocarcinoma, intrahepatic, previously treated, unresectable locally advanced or metastatic: Treatment of previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma harboring fibroblast growth factor receptor 2 gene fusions or other rearrangements in adults. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Opdualag (nivolumab/ relatlimab); 240mg/80mg per 20mL IV solution | Melanoma, unresectable or metastatic: Treatment of unresectable or metastatic melanoma in adult and pediatric patients ≥12 years of age. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Rezlidhia (olutasidenib); 150mg oral capsule | Acute myeloid leukemia, relapsed or refractory: Treatment of relapsed or refractory acute myeloid leukemia in adults with a susceptible isocitrate dehydrogenase-1 mutation as detected by an FDA-approved test. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Tecvayli (teclistamab); 10 mg/mL and 90 mg/mL IV solution | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults who have received at least 4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Commercial: Non Preferred Specialty Medical with PA; Reviewed by eviCore when applicable
Medicare: Part B; Reviewed by eviCore |
| Vonjo (pacritinib); 200mg oral capsule | Myelofibrosis: Treatment of intermediate or high-risk primary or secondary (postpolycythemia vera or postessential thrombocythemia) myelofibrosis in adults with a platelet count <50,000/mm3 | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
| Xalkori (crizotinib); 200mg and 250mg oral tablet | Inflammatory myofibroblastic tumor, ALK-positive, unresectable, recurrent, or refractory: Treatment of ALK-positive unresectable, recurrent, or refractory inflammatory myofibroblastic tumor in adult and pediatric patients ≥1 year of age. | Commercial: Non Preferred Specialty Pharmacy with PA; Reviewed by eviCore when applicable
Medicare: Part D; Tier 5, Rx Specialty with PA |
New Oncology Indications (could be Part B or D, depending on member)
| Drug | New Indication | Coverage |
| Brukinsa (zanubrutinib) | Lymphocytic lymphoma: treatment of adult patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Enhertu (fam-trastuzumab deruxtecan) | Breast cancer, unresectable or metastatic, HER2-low: Treatment of unresectable or metastatic HER2-low (immunohistochemical [IHC] 1+ or IHC 2+ and negative in situ hybridization [ISH-]) breast cancer (as determined by an approved test) in adults who have received a prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant therapy. | Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Ibrance (palbociclib) | Breast cancer, advanced (with disease progression following endocrine therapy): Treatment of HR-positive, HER2-negative advanced or metastatic breast cancer (in combination with fulvestrant) in adult patients with disease progression following endocrine therapy. | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Libtayo (cemiplimab) | Non–small cell lung cancer, locally advanced or metastatic:
First-line treatment (single-agent or in combination) of non–small cell lung cancer in adults whose tumors have high PD-L1 expression (Tumor Proportion Score ≥50%) as determined by an approved test, with no EGFR, ALK, or ROS1 aberrations, and with locally advanced (in patients who are not candidates for surgical resection or definitive chemoradiation) or metastatic disease. |
Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Nubeqa (darolutamide) | Prostate cancer, metastatic, hormone-sensitive: Treatment of metastatic hormone-sensitive prostate cancer (in combination with docetaxel) in adults. | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Tecentriq (atezolizumab) | Alveolar soft part sarcoma: treatment of adult and pediatric patients 2 years of age and older with unresectable or metastatic alveolar soft part sarcoma (ASPS). | Commercial: Non Preferred Specialty Medical with PA
Medicare: Part B |
| Tukysa (tucatinib) | Colorectal cancer: treatment of adult patients with RAS wild-type, human epidermal growth factor receptor 2 (HER2)-positive unresectable or metastatic colorectal cancer that has progressed following treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy in combination with trastuzumab | Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part D, Tier 5 Rx Specialty with PA |
| Xeloda (capecitabine) | Pancreatic adenocarcinoma: Adjuvant treatment of adults with pancreatic adenocarcinoma as a component of a combination chemotherapy regimen
Gastroesophageal junction adenocarcinoma: Treatment of adults with HER2-overexpressing metastatic gastric or gastroesophageal junction adenocarcinoma who have not received prior treatment for metastatic disease as a component of a combination regimen AND Treatment of adults with unresectable or metastatic gastric, esophageal, or gastroesophageal junction cancer as a component of a combination chemotherapy regimen |
Commercial: Non Preferred Specialty Pharmacy with PA
Medicare: Part B |
Infectious Disease
Formulary Additions
- Vivjoa (oteseconazole)—To reduce the incidence of recurrent vulvovaginal candidiasis (RVVC) in females with a history of RVVC who are not of reproductive potential, alone or in combination with fluconazole
- Formulary placement recommendations
- Commercial—Non-Preferred Brand with PA and MDL
- Medicare—Non-Formulary
- Formulary placement recommendations
- Rebyota (fecal microbiota, live-jslm)—For the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Medical with PA
- Medicare—Part B with PA
- Formulary placement recommendations
- Sunlenca (lenacapavir)—Treatment of HIV-1 infection, in combination with other antiretrovirals, in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy (oral tablet) or Medical (injectable)
- Medicare—Tier 5 Pharmacy Specialty
- Formulary placement recommendations
Commercial
Oncology/Hematology
Criteria Changes*
- Jakafi—Added criteria for chronic graft versus host disease
- Oxbryta—Updated criteria language, specified drug in quantity limit
- Promacta—Added coverage criteria for hepatitis C related thrombocytopenia
- Soliris—Updated coverage criteria to include REMS program and review by medical director, exclusion criteria and HCPCS code
- Ultomiris—Added criteria for Myasthenia Gravis, updated exclusion criteria
- Tavalisse—Added specialist and age criteria
Infectious Disease
Criteria Changes*
- Brexafemme (ibrexafungerp)—Added criteria for new indication RVVC, exclusion criteria
- Hepatitis B Treatment – Hepsera, Baraclude, Vemlidy & Pegasys—Added Pegasys to the policy, updated age criteria
- Pretomanid—Updated diagnosis and exclusion criteria
- Preventive Vaccine Policy—Added criteria for Dengvaxia, updated policy purpose and statement
- Sirturo (bedaquiline)—Added specialist and age criteria
Miscellaneous Criteria Changes*
- Diabetes Drug Therapies—Updated GLP-1/Mounjaro criteria, removed Adlyxin (discontinued)
- Rituxan, Ruxience, and Truxima (rituximab)—Added criteria for cold agglutinin disease
- Weight Loss Medications—Added approval period language
- NOTE: Only select Self-Funded plans currently cover weight loss medications.
- Non-Radiographical Axial Sponyloarthritis—Created policy that defines the criteria for coverage of immunomodulators used in the treatment of Non-radiographic Axial Spondyloarthritis (nr-axSpA) (currently Cimzia, Rinvoq Taltz, and Cosentyx under the Specialty Pharmacy benefit)
Commercial Tier Changes
Positive Changes
- Diazepam oral tablets and solution: Move from Non-Preferred Generic to Preferred Generic
- Brand Valium oral tablets: Move from Non-Preferred Brand to Preferred Brand
- Feedback from the market conduct exam requires alcohol withdrawal products be covered at Preferred status
Note: There were no negative changes.
* Members currently utilizing these therapies will not experience a disruption.
Please Note: The P&T Committee meets bimonthly, and formulary changes and criteria changes can occur during the meetings. Negative formulary changes are made effective on 1/1 and 7/1, while positive formulary changes are effective immediately to better serve our members and providers. Drug coverage and policies in the following categories will be reviewed during the remainder of 2023 and changes may be made:
- April Meeting: Rheumatology, Gastroenterology, Dermatology.
- June Meeting: Cardiology, Endocrinology, Pulmonology.
- August Meeting: Neurology, Psychiatry, Pain.
- October Meeting: Ophthalmology, Urology, Rare Diseases.
- December Meeting: Specialty and Medicare.
Reid – Pharmacy Updates
Medicare
Oncology/Hematology
Formulary Additions
- Enjaymo (sutimlimab-jome)—Used to decrease the need for red blood cell transfusion due to hemolysis in adults with cold agglutinin disease
- Formulary placement recommendations
- Medicare—Part B with PA
- Formulary placement recommendations
- Pyrukynd (mitapivat)—Treatment of hemolytic anemia in adults with pyruvate kinase deficiency
- Formulary placement recommendations
- Medicare—Non-Formulary
- Formulary placement recommendations
- Vijoice (alpelisib)—Treatment of severe manifestations of PIK3CA-related overgrowth spectrum in patients ≥2 years of age who require systemic therapy
- Formulary placement recommendations
- Medicare—Non-Formulary
- Formulary placement recommendations
- Hemgenix (etranacogene dezaparvovec)—Treatment of hemophilia B (congenital factor IX deficiency) in adults who currently use factor IX prophylaxis therapy, or have current or historical life-threatening hemorrhage, or have repeated, serious spontaneous bleeding episodes
- Formulary placement recommendations
- Medicare—Part B with PA
- Formulary placement recommendations
- Zynteglo (betibeglogene autotemcel)—Treatment of beta thalassemia in adult and pediatric patients who require regular red blood cell transfusions
- Formulary placement recommendations
- Medicare—Not Covered
- Formulary placement recommendations
| New Oncology Drug | Indication | Coverage Recommendation |
| Adstiladrin (nadofaragene firadenovec-vncg); gene therapy | Bladder cancer: Treatment of adult patients with high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors. | Medicare: Part B; Reviewed by eviCore |
| Carvykti (ciltacabtagene autoleucel); CAR-T 100000000 cells | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults after ≥4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Medicare: Part B; Reviewed by eviCore |
| Elahere (mirvetuximab soravtansine); 100 MG/20ML IV solution | Epithelial ovarian, fallopian tube, or primary peritoneal cancer, folate receptor-alpha positive, platinum-resistant: Treatment of folate receptor-alpha positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer in adults, who have received 1 to 3 prior systemic treatment regimens. Select patients for therapy based on an FDA-approved test. | Medicare: Part B; Reviewed by eviCore |
| Imjudo (tremelimumab); 300 mg/15 mL and 25 mg/1.25 mL IV solution | Hepatocellular carcinoma, unresectable: Treatment of unresectable hepatocellular carcinoma (in combination with durvalumab) in adults. | Medicare: Part B; Reviewed by eviCore |
| Kimmtrak (tebentafusp); 100 mcg/0.5 mL IV solution | Uveal melanoma, unresectable or metastatic: Treatment of HLA-A*02:01-positive unresectable or metastatic uveal melanoma in adults. | Medicare: Part B; Reviewed by eviCore |
| Krazati (adagrasib); 200mg oral tablet | Non–small cell lung cancer, locally advanced or metastatic, KRAS G12C-mutated: Treatment of KRAS G12C-mutated locally advanced or metastatic non–small cell lung cancer (NSCLC), as determined by an approved test, in adults who have received at least 1 prior systemic therapy. | Medicare: Part D; Tier 5, Rx Specialty with PA |
| Lunsumio (mosunetuzumab-axgb); 1mg/mL IV solution | Follicular Lymphoma: Treatment of adult patients with relapsed or refractory (R/R) follicular lymphoma (FL) after two or more lines of systemic therapy | Medicare: Part B; Reviewed by eviCore |
| Lytgobi (futibatinib); 4mg oral tablet | Cholangiocarcinoma, intrahepatic, previously treated, unresectable locally advanced or metastatic: Treatment of previously treated, unresectable, locally advanced or metastatic intrahepatic cholangiocarcinoma harboring fibroblast growth factor receptor 2 gene fusions or other rearrangements in adults. | Medicare: Part D; Tier 5, Rx Specialty with PA |
| Opdualag (nivolumab/ relatlimab); 240mg/80mg per 20mL IV solution | Melanoma, unresectable or metastatic: Treatment of unresectable or metastatic melanoma in adult and pediatric patients ≥12 years of age. | Medicare: Part B; Reviewed by eviCore |
| Rezlidhia (olutasidenib); 150mg oral capsule | Acute myeloid leukemia, relapsed or refractory: Treatment of relapsed or refractory acute myeloid leukemia in adults with a susceptible isocitrate dehydrogenase-1 mutation as detected by an FDA-approved test. | Medicare: Part D; Tier 5, Rx Specialty with PA |
| Tecvayli (teclistamab); 10 mg/mL and 90 mg/mL IV solution | Multiple myeloma, relapsed or refractory: Treatment of relapsed or refractory multiple myeloma in adults who have received at least 4 prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 monoclonal antibody. | Medicare: Part B; Reviewed by eviCore |
| Vonjo (pacritinib); 200mg oral capsule | Myelofibrosis: Treatment of intermediate or high-risk primary or secondary (postpolycythemia vera or postessential thrombocythemia) myelofibrosis in adults with a platelet count <50,000/mm3 | Medicare: Part D; Tier 5, Rx Specialty with PA |
| Xalkori (crizotinib); 200mg and 250mg oral tablet | Inflammatory myofibroblastic tumor, ALK-positive, unresectable, recurrent, or refractory: Treatment of ALK-positive unresectable, recurrent, or refractory inflammatory myofibroblastic tumor in adult and pediatric patients ≥1 year of age. | Medicare: Part D; Tier 5, Rx Specialty with PA |
New Oncology Indications (could be Part B or D, depending on member)
| Drug | New Indication | Coverage |
| Brukinsa (zanubrutinib) | Lymphocytic lymphoma: treatment of adult patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). | Medicare: Part D, Tier 5 Rx Specialty with PA |
| Enhertu (fam-trastuzumab deruxtecan) | Breast cancer, unresectable or metastatic, HER2-low: Treatment of unresectable or metastatic HER2-low (immunohistochemical [IHC] 1+ or IHC 2+ and negative in situ hybridization [ISH-]) breast cancer (as determined by an approved test) in adults who have received a prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant therapy. | Medicare: Part B |
| Ibrance (palbociclib) | Breast cancer, advanced (with disease progression following endocrine therapy): Treatment of HR-positive, HER2-negative advanced or metastatic breast cancer (in combination with fulvestrant) in adult patients with disease progression following endocrine therapy. | Medicare: Part D, Tier 5 Rx Specialty with PA |
| Libtayo (cemiplimab) | Non–small cell lung cancer, locally advanced or metastatic:
First-line treatment (single-agent or in combination) of non–small cell lung cancer in adults whose tumors have high PD-L1 expression (Tumor Proportion Score ≥50%) as determined by an approved test, with no EGFR, ALK, or ROS1 aberrations, and with locally advanced (in patients who are not candidates for surgical resection or definitive chemoradiation) or metastatic disease. |
Medicare: Part B |
| Nubeqa (darolutamide) | Prostate cancer, metastatic, hormone-sensitive: Treatment of metastatic hormone-sensitive prostate cancer (in combination with docetaxel) in adults. | Medicare: Part D, Tier 5 Rx Specialty with PA |
| Tecentriq (atezolizumab) | Alveolar soft part sarcoma: treatment of adult and pediatric patients 2 years of age and older with unresectable or metastatic alveolar soft part sarcoma (ASPS). | Medicare: Part B |
| Tukysa (tucatinib) | Colorectal cancer: treatment of adult patients with RAS wild-type, human epidermal growth factor receptor 2 (HER2)-positive unresectable or metastatic colorectal cancer that has progressed following treatment with fluoropyrimidine-, oxaliplatin- and irinotecan-based chemotherapy in combination with trastuzumab | Medicare: Part D, Tier 5 Rx Specialty with PA |
| Xeloda (capecitabine) | Pancreatic adenocarcinoma: Adjuvant treatment of adults with pancreatic adenocarcinoma as a component of a combination chemotherapy regimen
Gastroesophageal junction adenocarcinoma: Treatment of adults with HER2-overexpressing metastatic gastric or gastroesophageal junction adenocarcinoma who have not received prior treatment for metastatic disease as a component of a combination regimen AND Treatment of adults with unresectable or metastatic gastric, esophageal, or gastroesophageal junction cancer as a component of a combination chemotherapy regimen |
Medicare: Part B |
Infectious Disease
Formulary Additions
- Vivjoa (oteseconazole)—To reduce the incidence of recurrent vulvovaginal candidiasis (RVVC) in females with a history of RVVC who are not of reproductive potential, alone or in combination with fluconazole
- Formulary placement recommendations
- Medicare—Non-Formulary
- Formulary placement recommendations
- Rebyota (fecal microbiota, live-jslm)—For the prevention of recurrence of Clostridioides difficile infection (CDI) in individuals 18 years of age and older, following antibiotic treatment for recurrent CDI
- Formulary placement recommendations
- Medicare—Part B with PA
- Formulary placement recommendations
- Sunlenca (lenacapavir)—Treatment of HIV-1 infection, in combination with other antiretrovirals, in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection failing their current antiretroviral regimen due to resistance, intolerance, or safety considerations
- Formulary placement recommendations
- Medicare—Tier 5 Pharmacy Specialty
- Formulary placement recommendations
Please Note: The P&T Committee meets bimonthly, and formulary changes and criteria changes can occur during the meetings. Negative formulary changes are made effective on 1/1 and 7/1, while positive formulary changes are effective immediately to better serve our members and providers. Drug coverage and policies in the following categories will be reviewed during the remainder of 2023 and changes may be made:
- April Meeting: Rheumatology, Gastroenterology, Dermatology.
- June Meeting: Cardiology, Endocrinology, Pulmonology.
- August Meeting: Neurology, Psychiatry, Pain.
- October Meeting: Ophthalmology, Urology, Rare Diseases.
- December Meeting: Specialty and Medicare.
Contact Us
(800) 851-3379, option 3