Carle August Newsletter 2021
August 17, 2021Always at Your Side
As summer begins to turn into fall, we want to remind you that we’re always here for you – with information, resources, helpful tools and answers to any questions you may have. We know how hard you work keeping our members healthy, and we’re dedicated to always being there for you to help however we can. As always, reach out to your provider relations specialist and let us know what you might need, how we can help you and ways we can make your job easier. We’re grateful for all you do.
As It Relates to You
Provider Satisfaction Survey Coming Soon
We depend on you to take care of our members’ health, and we deeply value your opinion. Each year, we send provider satisfaction surveys to a random sample of our providers. We use the feedback from these surveys to make changes to our processes as part of our effort of constant improvement. If you receive a survey, please take the time to give us your honest feedback. It’s how we’re best able to adapt and meet your current and future needs.
We thank you in advance for your help with the survey and – as always – for the excellent care you give our members.
Provider Portal Improvements – and More!
As mentioned above, we lean on you to give us honest advice about how we can make our services, processes and communication better. Thanks to your feedback, we’ve made some great changes to our Provider Portal and beyond. Please see this PDF, which highlights just some of the recent updates and improvements we’ve made.
If you have any questions, please do not hesitate to reach out to your provider relations specialist. You work hard to help keep our members healthy. We want to make your job as easy as possible – giving you resources, removing roadblocks and always being available to answer your questions. Thank you for your partnership and your advice. We’ll continue to listen.
REMINDER: New Appeals Process
To maintain an organized and thorough provider appeals process, we continually review our own process efficiency as well as that of our provider community, and we also review the timeliness of appropriate resolutions.
As a result of this extensive review, we’ve decided to update our appeals process for physicians, healthcare professionals and facilities. For dates of service August 1, 2021, and after, the appeals process will now have one level of formal appeal after first asking for an informal inquiry on a denied claim. Both informal and formal appeals will need to be entered on our online Provider Inquiry Portal located at Provider.HealthAlliance.org. Please note, requests to obtain an appeal due to lack of prior authorization will only be granted for extenuating circumstances described in the informal inquiry request.
The purpose of an appeal is to escalate a reprocessing inquiry decision or bring immediate attention to a critical issue. An appeal should not be the first attempt at communication between the parties for any given issue. You may only appeal for specific reasons outlined in your provider agreement. These include contractual allowances, investigational services, clinical editing, no prior authorization and other specific reasons.
We’ll always try to resolve provider-initiated inquiries through the course of normal operational interactions and our informal inquiry resolution process. Providers must initiate informal inquiries within 90 days of the original denial. To clarify, we define provider informal inquiries as the first contact initiated by the provider to our staff. We accept these inquiries through our Provider Inquiry Portal. To ensure your initial inquiry is handled in the most timely manner, please provide as much detail as you can for why an appeal of the denied claim is being pursued.
If you’re not satisfied with the claims processing, administrative determination or outcome of the online claims reprocessing inquiry, as mentioned above, you may submit a formal appeal to us within 90 days from the original denial, unless otherwise stated in your contract. To submit a formal appeal, you must complete the Provider Appeal form located at Provider.HealthAlliance.org.
If you have any questions regarding the appeals process, please contact your provider relations specialist. We’re always happy to help. And thank you for all you do, every day, to keep our members healthy and well.
The “Big Six” – Vascular Disease
Supporting documentation and accurate coding are key to making sure your patients receive the care they need. Failure to document chronic conditions on an annual basis impacts your patients, fellow providers and our organization. Here are some helpful documentation and coding tips for Vascular Disease, one of the “Big Six” diagnosis categories frequently miscoded or unsupported in documentation.
Your documentation should include:
- Underlying cause and any manifestations.
- Link between the disease, its causation and any manifestation – using language like “due to” or “secondary to.”
- Type of vessel, whether it’s native or a graft. Identify whether grafts are autologous, non-autologous biological or non-biological.
- Laterality.
- Complications such as rest pain, skin ulcers or gangrene.
When medical surveillance for an aneurysm is prescribed, evaluate and report the aneurysm yearly and include its location and size.
For patients with chronic deep vein thrombosis (DVT) be sure to note:
- Chronicity
- Cause
- Treatments
- Location
A “history of DVT” should be reported after it’s resolved, even when the patient receives prophylactic treatment.
Finally, be sure to document any risk factors for your patient’s vascular disease – such as obesity, tobacco use, hypertension or diabetes, and include outcomes like amputations.
For short videos regarding all of the “Big Six” conditions – click here. Visit our Coding Counts page for even more helpful tips and resources. Thank you for your continued hard work and attention to detail.
A Helpful Reminder – Member Appeal Rights
We know there’s so much to remember, and sometimes it’s just best to have links at-hand to know where to look for important information. With that in mind, we wanted to remind you where you can find helpful information about our members’ rights, including their rights to appeal. Visit these links below to see the rights we give your patients who are members of our plans – and what role you play as the provider, particularly during complaints and appeals.
Commercial Members – Rights, Responsibilities and Appeals Procedures
Medicare Members – Rights and Responsibilities
Medicare Members – Appeals Procedures
This and much more can be found in our full provider manuals, linked here for easy reference.
Help Us Move the Needle
We Need You This Flu Season
This year – like last – it’s of increased importance that people in our communities get their yearly flu shot. With the COVID-19 pandemic still among us, we need to be doing all we can to recommend both the flu and COVID-19 vaccines. According to the CDC, recommendations – and even simple reminders – from their trusted providers are a critical factor in whether many adults get vaccines for themselves and their families.
With this in mind, the CDC is leading a SHARE campaign to urge providers to do all they can to encourage their patients to get their yearly flu shot. Here are the basics, directly quoted from their campaign:
- S – Share the reasons why the influenza vaccine is right for the patient given his or her age, health status, lifestyle, occupation or other risk factors.
- H – Highlight positive experiences with influenza vaccines (personal or in your practice), as appropriate, to reinforce the benefits and strengthen confidence in influenza vaccination.
- A – Address patient questions and any concerns about the influenza vaccine, including side effects, safety and vaccine effectiveness in plain and understandable language.
- R – Remind patients that influenza vaccines protect them and their loved ones from serious influenza illness and influenza-related complications.
- E – Explain the potential costs of getting influenza, including serious health effects, time lost (such as missing work or family obligations) and financial costs.
Each patient is different, and you know them best. Consider the best approach that’ll let them know just how important the flu vaccine is and why they and their families should get it. With your help, our communities can stay safer – and breathe easier – this flu season. Thanks for your help in this vital endeavor.
It varies according to health plan, but flu shots are covered at no cost to our members in most cases. Your patients can call the number on the back of their health plan member ID card to learn more about costs and where they can go to get their shots.
Substance Use Disorder
If you’ve watched the headlines lately, or even over the past two decades, you’ve probably realized how much of a problem substance use disorder (SUD) is in the U.S. Alarmingly, SUD has again increased over the last year during the COVID-19 pandemic. The good news – SUD is among the most preventable causes of mortality and morbidity, and appropriate screenings and treatments can act as interventions to improve outcomes for people experiencing unhealthy use. The U.S. Preventive Services Task Force (USPSTF) recommends that all adults be screened for unhealthy use in the primary care setting at least once a year. If unhealthy use is identified, it’s important to undergo a brief counseling intervention if warranted. If the unhealthy use is significant, a brief counseling session may not be enough for your patient.
Nearly 28% of American adults have an “unhealthy use” rate of alcohol, defined as the spectrum of use that can result in health consequences. More specifically, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) estimates “unhealthy use” as (on average) these amounts of alcohol:
- For men under 65: more than 14 drinks/week or over 4 drinks/day.
- For women of all ages, and all adults 65 and over: more than 7 drinks/week or over 3 drinks/day.
Nearly 18% of American adults have reported illicit drug use. There’s no set standard for what defines “unhealthy use” of illicit drugs, but many drugs can result in catastrophic outcomes with just a single use. For example, cocaine can cause myocardial infarction and injections can expose a person to HIV or other serious diseases.
Screening for unhealthy alcohol and drug use includes using brief, simple questions from validated tools. Many of these tools are specifically built for the particular healthcare setting in which they’re being used.
- Examples of questionnaires used for unhealthy alcohol use screening include single-item, AUDIT, AUDIT-C and CAGE.
- Examples for unhealthy drug use screening include single-item, DAST, SoDU and ASSIST.
- Screening tools that assess for both drug and alcohol use include CAGE AID, ASSIST, SUBS, TAPS and TAPS-1.
- Screening tools to detect SUD in pregnancy include T-ACE, Net, 4Ps Plus and TWEAK.
- Older adults can be screened for SUD with G-MAST and CARET.
- Adolescent screening for SUD may be accomplished with the CRAFFT tool.
If the screening is positive for unhealthy use, a full substance use assessment is recommended as a follow up. This should include a physical exam, review of systems and thorough medical history review. The DSM-V will assist to properly diagnose the patient. The level of intervention should then be determined, to get the patient the help that best fits their needs and circumstances. With this help, hopefully they can beat the issue and live a healthy life.
Source for this article: Richard Saitz, Screening for Unhealthy Use of Alcohol and Other Drugs in Primary Care, UpToDate, 2020.
Make Sure Patients Get Their Diabetic Eye Exams
Researchers have found that nearly 60% of Americans with diabetes don’t get their annual diabetic eye exam. How can you help change this discouraging stat? Sometimes the best medical tools are simple reminders and encouragement. Whenever your patients with diabetes come in for their annual wellness visit or physical:
- Remind them to schedule their annual diabetic eye exam.
- Offer encouragement, and remind them that 90% of the blindness caused by diabetes is preventable.
- Let them know that common eye diseases caused by diabetes often have no warning signs, and that a dilated/retinal eye exam is the best way to detect these diseases in their early stages.
- Remind them to have the ophthalmologist/optometrist send their eye exam results to their primary care provider if they get the exam at a different facility. You can even give your patients their PCP’s business card, for them to give to their ophthalmologist/optometrist.
- Ensure that they schedule their other diabetic preventive screenings they’re due for as well.
As their trusted provider, you can urge more people to take care of their health and well-being by getting the exams they need. Thank you for your help.
What To Know About Diabetic Retinopathy
As the above article points out, vision problems caused by diabetes are serious – and together we can help people catch issues early and treat problems if they arise. In addition to encouraging your patients with diabetes to get their yearly eye exam, here’s what you can do as their trusted provider:
- Give them educational information about diabetic retinopathy and diabetic macular edema, two common eye problems that can lead to serious vision loss and even blindness.
- Encourage your patients to maintain control of their blood sugar and blood pressure levels, as this can help prevent worsening vision problems caused by diabetic retinopathy.
- Most importantly – through their yearly exams and other checkups – keep a close watch on the health of your patients’ eyes. Early detection and treatment of diabetic retinopathy, followed by regular and consistent monitoring of its progression makes all the difference. In short, here’s what you should do, for all your patients with diabetes:
- You, your patients and their eye specialists should watch for early signs of diabetic retinopathy. People with diabetes usually don’t notice any symptoms or vision changes in the early stages, which makes the eye exams incredibly important. Doctors can use the Early Treatment Diabetic Retinopathy Study–Diabetic Retinopathy Severity Scale (ETDRS-DRSS, found here on page 3 and here with helpful images) to help detect the condition early.
- As soon as warning signs or diabetic retinopathy itself is detected, refer the patient for treatment.
- Regularly and consistently monitor the progression of your patient’s diabetic retinopathy. You and/or their eye specialist can again use the ETDRS-DRSS linked above to track progression.
- Stay abreast of the recommended treatments for all stages of the condition, and make timely referrals for these treatments as needed.
Diabetic retinopathy affects many people. But the good news is that early detection and treatment, followed by consistent monitoring and treatment of the condition’s progression, can help save your patients’ vision.
Sources for above article: Regeneron Pharmaceuticals, Inc., Diabetic Retinopathy and Diabetic Macular Edema: Quick Reference Guide and the Centers for Disease Control and Prevention.
Low Back Pain – Important Information About Imaging
Together we can help improve the health, well-being and care of your patients with low back pain (LBP). One way to do so is to avoid diagnostic imaging whenever it’s not needed. Here’s the important information you should know about the Healthcare Effectiveness Data and Information Set (HEDIS®) measure for the use of imaging studies for LBP.
Why Imaging Isn’t Always the Right Option
According to the National Committee for Quality Assurance (NCQA), which manages HEDIS, evidence has shown that unnecessary or routine imaging (X-ray, MRI, CT scans) for low back pain does not improve outcomes – and it also exposes patients to unneeded harms like radiation and further unnecessary treatments.
Therefore, avoid imaging for patients with LBP when there’s no indication of an underlying condition.
The HEDIS Measure
HEDIS looks at patients age 18 to 50 with a primary diagnosis (first diagnosis on a claim) of uncomplicated low back pain, in any of these healthcare settings:
- Office visits, outpatient evaluations, emergency department visits, observation level of care, telehealth/telemedicine visits, telephone visits, e-visits or virtual check-in visits.
- Physical therapy and/or osteopathic and/or chiropractic manipulative treatment.
It measures how many of these patients did and did not have an imaging study within 28 days of diagnosis. Knowing that each patient is unique and imaging is definitely required in some situations, HEDIS takes into account a large number of medical conditions where imaging might be medically necessary. If your patient has one of these conditions – and you note it in your evaluation – they can get imaging and it won’t negatively impact the HEDIS scores or your performance for NCQA.
The Most Important Take-Aways
- Don’t order diagnostic imaging for a patient in the first four weeks of new-onset low back pain, unless there are red flags or indications of an underlying condition.
- If your patient with low back pain does have an underlying condition where imaging might be medically necessary, always note this.
- Diagnostic imaging should only be ordered when necessary, because of the high occurrence of radiologic abnormalities in asymptomatic patients.
Recommended Routine Treatment for LBP
Finally, we’ll close with types of routine treatment for low back pain that we do recommend:
- Physical therapy – including stretching, massage, strengthening exercises and manipulation.
- First-line drug therapy with acetaminophen, a cyclo-oxygenase-2 inhibitor or a nonsteroidal anti-inflammatory drug.
- Steroidal drugs to reduce inflammation.
- Acupuncture (now covered for back pain treatment by many of our plans).
- Comorbid conditions like anxiety, depression or sleep disorders should be treated, and psychosocial issues should be addressed.
- Adjuvant antidepressants and anticonvulsants should be considered.
Thank you – as always – for the exceptional and compassionate care you give our members.
Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents
Another important HEDIS measure helps in the fight against childhood obesity. The WCC measure – short for Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents – looks at whether or not children age 3 to 17 receive body mass index (BMI) assessment and counseling for nutrition and physical activity during their checkups.
Why It Matters
As the NCQA notes, childhood obesity has more than doubled in children and tripled in adolescents in the past 30 years. It has both immediate and long-term health effects – and is the main health concern among parents in the U.S. Obesity can become a lifelong health issue, so it’s vital to deal with it early in life.
Details and Specifics
Here’s what you need to know about the HEDIS measure:
- The BMI assessment and counseling can be rendered during a visit other than the regular well-child visit and still meet the HEDIS requirements – just make sure all the specified documentation is present. However, services specific to the assessment or treatment of an acute or chronic condition do not count toward the counseling for nutrition and physical activity indicators.
- BMI assessments must document height, weight and BMI percentile.
- The height, weight and BMI percentile in this assessment must come from the same data source. You cannot – for example – take a child’s height measurement from a past visit and a weight measurement from the current checkup.
- Telehealth/virtual visits are acceptable. So are member-reported biometric values when documented in the medical record.
- Documentation of nutrition counseling must include at least one of the following:
- Discussion of nutrition behaviors, such as eating habits or dieting behaviors.
- Documentation of types of food or meal frequency.
- Counseling or referral for nutrition education.
- Weight or obesity counseling.
- Member received educational materials on nutrition during a face-to-face visit.
- Anticipatory guidance for nutrition.
- Completed checklist indicating nutrition was addressed.
- Documentation of physical activity counseling must include at least one of the following:
- Discussion of current physical activity behaviors, such as exercise routine, participation in sports or exams for sports participation.
- Counseling or referral for physical activity.
- Member received educational materials on physical activity during a face-to-face visit.
- Anticipatory guidance specific to the child’s physical activity.
- Weight or obesity counseling.
- Completed checklist indicating physical activity was addressed.
Together we can stem the tide of childhood obesity. Follow the HEDIS guidelines – and encourage your patients to eat healthy and be active. Thank you.
Schizophrenia in Children and Adolescents:
Psychosocial Interventions
Schizophrenia affects people of all ages and makes up a large portion of the global healthcare burden, according to the World Health Organization. In children and adolescents, schizophrenia can be debilitating and life-altering if not managed properly. In this age group, schizophrenia impacts proper development and cognitive function. Although etiology is unclear, schizophrenia affects nearly 0.5% of the population – and 0.04% experience its onset during childhood.
Here are some more facts you should know – all are important to understand when reviewing potential interventions:
- Pathogenesis of schizophrenia includes substance use, trauma, social adversity, genetic vulnerability, obstetric complications and environmental factors.
- Common comorbidities that exist alongside schizophrenia include auditory processing deficits, ADHD, OCD, MDD, language disorders and deficits with executive function.
- Risk factors for schizophrenia include cannabis use, complications in obstetrics related to hypoxia events, other substance use and psychotic symptoms.
Antipsychotic medication is the first-line of treatment for schizophrenia. Research shows that medication therapy may not be sufficiently therapeutic for the disorder, and therefore psychosocial interventions should be added to the pharmacotherapy. Effective psychosocial interventions include CBT, community outreach, skills training, psychoeducation with patient and family, cognitive enhancement/remediation and therapeutic school. These psychosocial interventions prevent relapse, promote medication adherence, encourage autonomy for your patient and reduce the family’s stress while increasing the supportive environment.
Thank you for your dedication and commitment to getting your patients with schizophrenia the help they need.
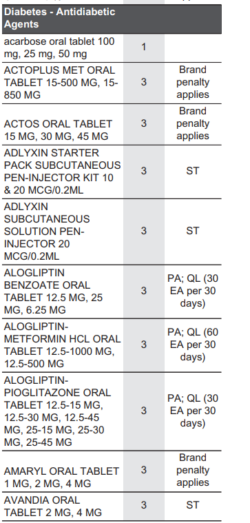
Pharmacy 101: How To Request a Brand-Name Drug When a Generic Is Available
As you know, generic medications – in most cases – cost less than their brand-name counterparts. The savings are passed on to our members, as most generics are covered at a tier 1 or tier 2 level of copay. That’s why most health plans require that if there’s a generic version of a brand-name drug available, the pharmacy dispense the generic.
However, if a provider or member requests a brand-name when a generic is available, there’s a process pharmacies can follow to move forward with dispensing the brand-name drug. Here’s how it works:
- The pharmacy must enter a DAW (dispense as written) code when processing the prescription.
- If the brand-name drug was requested by a provider, the pharmacy should use a DAW 1. If the request is from the member, the pharmacy should use a DAW 2.
- The use of these codes should bypass the insurance rejection stating that a generic must be dispensed.
- For any processing concerns, the pharmacy or provider can call our Customer Solutions team.
However, please always be aware that when a pharmacy dispenses a brand-name drug and a generic is available, the member will pay more. Most plans will add what’s called a “brand-name penalty” to the member’s copay. The penalty is the difference of cost between a brand-name medication and its equivalent generic. This amount can be quite significant. This penalty is not assessed on medications with a narrow-therapeutic-window – an example being Synthroid (brand levothyroxine).
Brand-name medications are usually considered “non-formulary” on Medicare plans. For a brand-name “non-formulary” medication to be covered (on a Medicare plan or on any plan), the provider must submit for a formulary exception indicating medical necessity. The list of medications, brand-name and generic, that are formulary is listed on the formulary document that’s linked to a member’s plan.
We encourage providers to have discussions with members requesting brand medications when a generic exists. Patients may benefit from education and reassurance that generics substituted by the pharmacy are interchangeable and proven equally efficacious to the brand by the FDA. The use of brands when a generic exists can increase member cost share and for Medicare members place them in the gap or “donut-hole” earlier in the year.
If you have any questions or concerns about what drugs are covered or require prior authorization, please call: Health Alliance Customer Solutions at (800) 851-3379; or Health Alliance Northwest Member Services at (877) 750-3350; or Health Alliance Medicare Member Services at (800) 965-4022. We’re always happy to help.
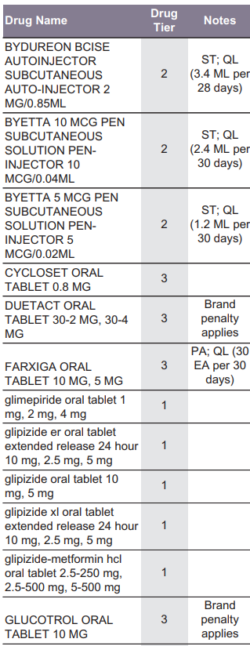
Pharmacy 101: What To Know About Formulary Alternatives
When a medication requires prior authorization (PA) or step therapy (ST) and the requirements aren’t met, it’ll result in a denial of coverage. However – when appropriate – the denial letter sent to the member and provider will also list formulary alternatives. Often, these are preferred formulary alternatives available on a lower tier – resulting in a cost savings to the member.
Some formulary alternatives may not require prior authorization, and the provider can prescribe without resubmitting to our pharmacy department. When the preferred formulary alternative does require prior authorization, the provider will have to submit a request (along with the required documentation) for a determination to be made.
The formulary lists medications by categories or classes, which can be reviewed by the provider to find a preferred formulary alternative for the member. The notes column will indicate whether PA or ST is required for the medication.
Pharmacy Updates
All Plans
Allergy / Immunology
Formulary Additions
- Orladeyo (berotralstat)—Prophylaxis to prevent attacks of hereditary angioedema (HAE) in adults and pediatric patients 12 years and older
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA
- Medicare—Tier 5 with PA
- Formulary placement recommendations
Cardiology
Formulary Additions
- Evkeeza (evinacumab)—Indicated as an adjunct to other low-density lipoprotein cholesterol (LDLC)–lowering therapies for the treatment of adult and pediatric patients, aged 12 years and older, with homozygous familial hypercholesterolemia (HoFH)
- Formulary placement recommendation s
- Commercial—Tier 6 with PA
- Medicare—Non-Formulary
- Formulary placement recommendation s
- Verquvo (vericiguat)—Indicated to reduce the risk of cardiovascular death and heart failure (HF) hospitalization following a hospitalization for HF or need for outpatient intravenous (IV) diuretics in adults with symptomatic chronic HF and ejection fraction less than 45%
- Formulary placement recommendations
- Commercial— Non-Preferred Brand with PA
- Medicare—Non-Formulary
- Formulary placement recommendations
Endocrinology
Formulary Additions
- Isturisa (osilodrostat)—Treatment of adult patients with Cushing’s disease (CD) for whom pituitary surgery is not an option or has not been curative
- Formulary placement recommendations
- Commercial—Non-Preferred Specialty Pharmacy with PA
- Medicare—Tier 5 with PA
- Formulary placement recommendations
Pulmonology
Formulary Additions
- Bronchitol (mannitol)—Indicated as add-on maintenance therapy to improve pulmonary function in adult patients 18 years of age and older with cystic fibrosis
- Formulary placement recommendations
- Commercial—Tier 6 with PA
- Medicare—Non-Formulary
- Formulary placement recommendations
Commercial
Tier Changes
Commercial Tier Changes
- Breztri Aerosphere—Move from Non-Preferred Brand to Preferred Brand
- Triple therapy inhaler option
- Covered in parity with Trelegy
- Lonhala—Move from Excluded to Non-Preferred Specialty with PA (policy presented above)
Cardiology
New Policies
- Farxiga Non-Diabetes Indications
- Provides criteria for coverage of Farxiga for heart failure and chronic kidney disease
- Farxiga is currently a Non-Preferred SGLT2 inhibitor for diabetes
Criteria Changes
- Weight Loss Medications
- Added contraindication
Retired Policies
- PCSK9 Inhibitors
- Other health plans are beginning to remove PAs on these agents
- Providers have largely been using statins as first-line treatment
- High approval rate
Endocrinology
New Policies
- Oriahnn (elagolix, estradiol, and norethindrone)—Treatment of heavy bleeding associated with uterine fibroids
- Line extension for Orilissa (elagolix)
Criteria Changes
- Leuprolide Acetate
- Updated language regarding surgery for uterine fibroids
- Added requirement that patient not be concurrently taking Oriahnn
- Erectile Dysfunction Medications
- Operational update to accommodate those FCC Self-Funded plans that have a custom MDL of #6 tablets per 30 days
Pulmonology
New Policies
- Lonhala Magnair
- Moving from Excluded to Non-Preferred Specialty Pharmacy with PA to capture rebates
- Member must have COPD and step through LAMA inhaler
Criteria Changes
- Actemra (tocilizumab)
- Added criteria for Systemic Sclerosis-Associated Interstitial Lung Disease (SSc-ILD)
- Esbriet (pirfenidone) and Ofev (nintedanib esylate)
- Updated language for SSc-ILD
- Kalydeco (ivacaftor), Symdeko (tezacaftor-ivacaftor), Trikafta (elexacaftor-tezacaftor-ivacaftor)
- Added list of qualifying mutations to each policy
- Xolair (omalizumab)
- Added Xolair prefilled syringe to policy
- Added criteria for rhinosinusitis nasal polyposis, which includes step through preferred product, Dupixent.
- Yupelri
- Removed specialist requirement
- Changed step requirement from two to one LAMA