February Newsletter
February 4, 2014Happy New Year!
We’re gearing up for another great year of partnership with each of you, and we appreciate your hard work and dedication to your patients and our members. As always, your provider relations specialist will be there for you throughout 2014 if you have any questions or concerns. They act as a liaison between us to help with open communication.
One of our accomplishments last year was that our provider relations staff visited approximately 2,000 provider offices. These visits involved educating providers on our policies and procedures, our new plans and products, Clear Coverage training, and more. Sometimes it was just checking in to see how things were going.
If you would like to set up a meeting, call your provider relations specialist. We look forward to meeting with you soon!
Request Preauthorization through Your Health Alliance
We appreciate your feedback on our annual provider satisfaction survey. One area we want to address is the referral and preauthorization submission process.
We introduced Clear Coverage, an automated preauthorization process, in 2010. It allows you to submit an authorization request for some tests and procedures that result in real-time response to approved requests. Providers who use the Clear Coverage system have reported satisfaction with the program. However, not all preauthorization requests can be submitted through Clear Coverage.
In the past, requests that can’t go through Clear Coverage have been submitted via fax. We’ve implemented an online preauthorization form that you can use through Your Health Alliance* for providers and office managers. We believe the online form will be easier and more efficient than faxing.
The form, with any associated documentation, is completed online and submitted via the secure website. This electronic format enhances management of preauthorization requests and gives you confirmation that the request has been received. It also allows you to track the preauthorization process.
You can find a guide for using Your Health Alliance and a Clear Coverage tutorial under Forms and Resources once you’ve logged it.
Requests that don’t qualify for immediate approval are pended for review. If the request is for urgent care**, the review is completed within 24 hours if all requested information is received. All other types of requests and submission are processed within 5 to 7 days if all information is received with the request. If you prefer, you can continue to send preauthorization requests via fax.
If you have questions about the preauthorization process or any of the methods available to submit a preauthorization request, please contact your provider relations specialist.
*You need to register for an account the first time you visit Your Health Alliance.
**Urgent care means medical care or treatment where using the timetable for a non-urgent care determination could seriously jeopardize the patient’s life/health or the patient’s ability to regain maximum function or, in the opinion of the attending or consulting physician, would subject the patient to severe pain that could not be adequately managed without the requested care or treatment.
HEDIS® Chart Reviews Draw Near
Each spring, we collect data to determine how we measure up against national averages for the Healthcare Effectiveness Data and Information Set (HEDIS). This data collection and analysis indicates where we need to focus our quality efforts and is required to obtain National Committee for Quality Assurance (NCQA) accreditation. Successfully completing our HEDIS report depends largely on the cooperation we receive from provider office staff. In other words, we need your help.
Gathering data for the HEDIS audit requires access to medical records. Random samples are generated for each HEDIS measure. If your office is identified in one or more sample, you may receive a request by mail or fax asking you to copy and send specific medical records to us or a representative may visit your office to review and collect copies of specific medical records relating to HEDIS.
The HEDIS audit is overseen by an external audit group to ensure compliance to standards and specifications. Our reviewers are professionals who understand the importance of personal health information. All individually identifiable information concerning patients will be kept strictly confidential in compliance with HIPAA regulations.
You can learn more about HEDIS in the provider manual in the Forms and Resources section of Your Health Alliance. HEDIS results are posted on HealthAlliance.org.
If you have any questions about HEDIS, contact our Quality Management Department at 1-800-851-3379, extension 8112.
HEDIS Breast Cancer Screening Measure
The U.S. Preventive Services Task Force recommends women 50-74 years old have a mammogram every 2 years. Biennial screening is a personal decision for women 40-49 years old.
Beginning with HEDIS 2014, NCQA will also include women age 50-74 in the Breast Cancer Screening measurement. NCQA also requires one or more mammograms every 2 years. HEDIS does not consider breast biopsies, ultrasounds, or MRIs as appropriate methods for primary breast cancer screening.
Please keep these guidelines in mind when recommending testing to your patients.
Note: Some mammography centers require referrals from the health care provider and will not accept self-referrals from the patient.
HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).
ICD-10 is Coming this October
ICD-10 will be implemented on October 1, 2014, replacing ICD-9. The health care system as a whole will benefit from more choices in the code sets to help categorize conditions with greater specificity. More defined codes will allow for laterality for conditions such as ulcers and fractures. Other conditions that may have required multiple codes in ICD-9 may only need one code in ICD-10. Some descriptors of conditions will not be required in ICD-10, such as the omission of malignant, benign and unspecified for essential hypertension.
Please assess whether you are ready for ICD-10. If you aren’t, talk to your administrators and ask them what your plan for ICD-10 is. You can also view the official CMS Industry Resources for the ICD-10 transition at the CMS website. Plus, stay tuned to your email for the new ICD-10 Sneak Peek from Coding Counts, brought to you by our Risk Management coding consultant team.
If you would like to make sure you are on the Coding Counts email distribution list, email us at CodingCounts@healthalliance.org.
Reminder about In-Network Referrals
Remember to use contracted in-network providers before referring a patient outside our network. You can search a member’s network on Your Health Alliance for providers and office personnel by attaching to that member.
Meet with our Coding Consultant Team
Our high-volume participating providers met with the new members of our Risk Adjustment Coding Consultant team in the last quarter. The team will soon be scheduling a new round of meetings for 2014. The team is happy to discuss any coding or quality questions you may have or to provide member-specific examples.
If you’re interested, email us at CodingCounts@healthalliance.org. And don’t forget to check out the coding team blog, Coding Counts.
Grace Period on Premium Payments
The Affordable Care Act (ACA) gives those members who were approved for a subsidy a 90-day grace period to pay their premiums. Meanwhile, we are obligated to pay on claims during this period. If a member defaults during the end of 90 days, the state will notify us and we will recoup any payments made on these members according to the refund policy in your contract.
Online Provider Satisfaction Survey Coming Soon
Each year, we send provider satisfaction surveys to a random sample of Health Alliance providers. We take the feedback from these surveys seriously and value your input as we continue to improve our processes.
This year, we are doing things a little differently and sending out the surveys through email. If you receive a survey, please take the time to give us your honest feedback. If your office does not have internet access and would like to receive a paper survey, contact your provider relations specialist. Thanks in advance for completing the survey, and for the excellent care you provide our members, your patients.
Order Quit For Life® Materials
We have tear-off pads and fliers available for the new Quit For Life smoking cessation program. If you would like to receive these materials, please contact your provider relations specialist or Penny Shaw at 217-337-3409 or Penny.Shaw@healthalliance.org.
2014 Provider Manuals
The 2014 Health Alliance Provider Manual will soon be available on Your Health Alliance for providers and office personnel. If your office doesn’t have internet access, you may request a CD copy of the manual by contacting your provider relations specialist.
Pharmacy
Medicare
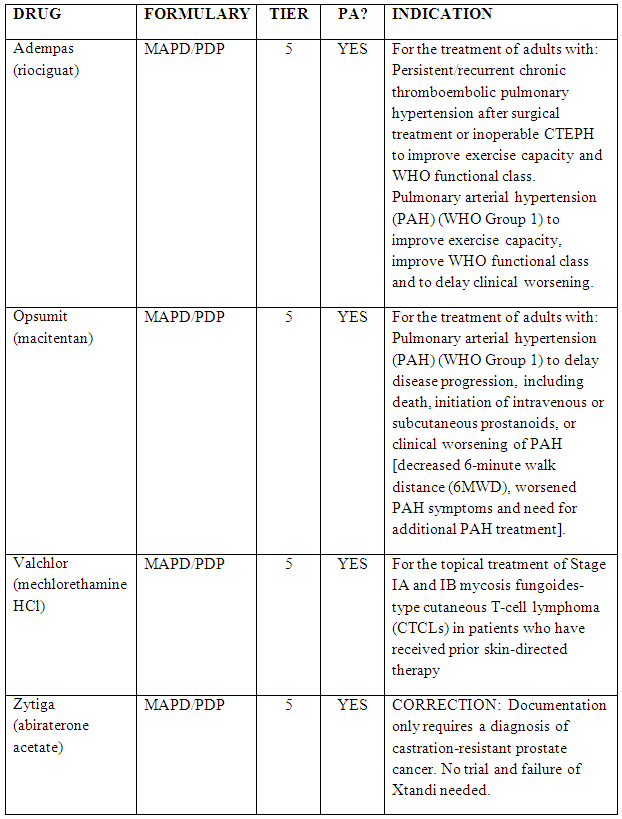
2014 Formulary Changes
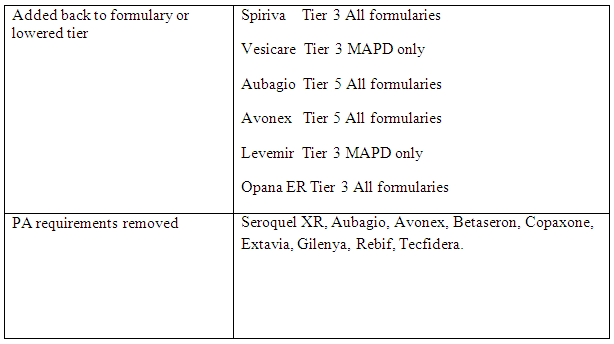
New and Revised Policies
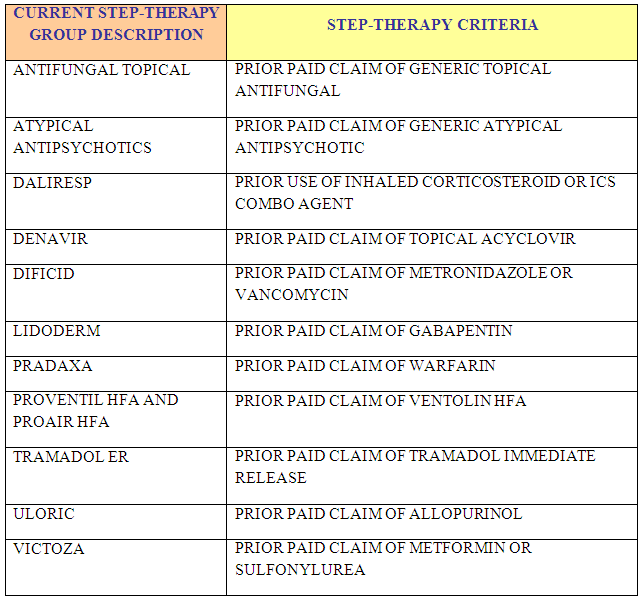
New Step Edits
Commercial
Formulary Additions
- Diclegis (doxylamine succinate/pyridoxine hydrochloride) – Tier 3
- Procysbi (cysteamine bitartrate delayed-release capusules) – Tier 6 with preauthoriation (PA)
- Breo Ellipta (fluticasone furoate and vilanterol trifenatate inhalation powder) – Tier 3 with Step Therapy edit
Formulary Exclusions
- Oxytrol will be excluded, but is now available over the counter
Drugs With New Restrictions
- Zyvox (linezolid) coverage limited to select infections caused by antibiotic-resistant gram positive bacteria
Drugs Moving to Tier 3 – Effective 2/1/14
- Seroquel XR (quetiapine fumarate)
- Protopic (tacrolimus)
- Pulmicort (budesonide)
Specialty Drugs Moving Tiers – Effective 1/1/2014
- Remicade – Moving from Preferred Specialty Medical (Tier 4) to Non-preferred Specialty Medical (Tier 5)
- Cimzia – Moving from Non-preferred Specialty Pharmacy (Tier 5) to Preferred Specialty Pharmacy (Tier 4)
Preauthorization Criteria Updates
- Remicade Preauthorization Requirements
- Trial and failure, contraindication, or intolerance to Cimzia, Humira and Enbrel
- Patients will have to try and fail these medications when appropriate, based on indication being treated
- Cimzia – No longer requires a trial and failure of the previous preferred products Remicade, Enbrel, and Humira