FLASH: Enhanced IVR Features for You and Our Members
September 19, 2019We’re excited to share that we’ve upgraded our interactive voice response (IVR) phone system, allowing us to better serve your office and our members. To use the new system, call 1-800-851-3379, option 3. This will enable you to access the options specifically created for providers.
Please see the details below. If you have any questions, contact your provider relations specialist.
Provider Capabilities
Our new IVR system makes it easy for any of your office staff to quickly check the status of claims and preauthorization requests.
Claims Status
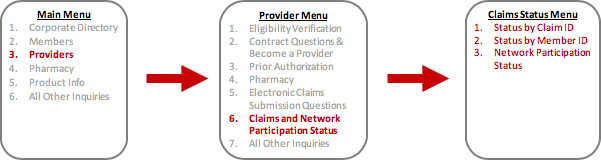
To use the new system, call 1-800-851-3379, option 3.
- Then, select prompt 6 to check if a claim has been received and when it was received. This IVR function can also tell you if the claim has been processed and when it was processed.
- There are a few options from this prompt:
- Claim Lookup by Claim ID: This path will collect the claim ID to provide information on the claim.
- Claim Lookup by Member ID: This path will collect the member’s ID and the date of service to provide information on the claim.
- Network Participation Status: This path will send callers directly to a representative.
- Callers must have either the claim ID or member number, date of service and dollar amount of the service (if there were multiple services performed on the same date).
Preauthorization Status
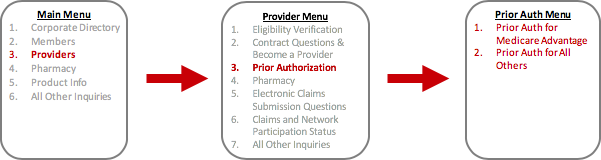
To use the new system, call 1-800-851-3379, option 3.
- Then, select prompt 3 again to see if preauthorization is needed for a certain procedure code based on a member’s plan. If preauthorization is needed, the IVR will tell you where (with which vendor) to start the preauthorization process.
- If a member’s plan does not allow a procedure at all, the system will tell you.
- If a member’s plan has a non-standard preauthorization list, you’ll be routed to a representative.
- Callers must have the member ID and procedure code. The current IVR doesn’t recognize the input of letters. If you’re asking about procedure codes that have a mixture of letters and numbers, you’ll be routed to a representative.
- You’ll receive a confirmation number for your records for completed inquiries. This confirmation number will be saved in the member’s record, and our representatives will be able to access this confirmation number, if there are future questions about it. Please have a pen ready when entering your request to capture the confirmation number from the IVR.
Note: The preferred method for checking the status of claims and preauthorization requests is still YourHealthAlliance.org for providers. We can provide more complete and detailed information through your portal.
Benefits of the new IVR system include:
- Reduced wait times to handle status checks on claims and preauthorization requests
- Improved consistency of response, meaning you’ll receive the same response whether you use the website, the IVR system or talk with a representative
- Automated creation of confirmation case numbers that will be placed in the member’s record
You’ll need to talk to a representative rather than use IVR if:
- For a preauthorization request, you’re checking on a procedure code that has a combination of numbers and letters
- You’re checking a claim status for a member who has multiple claims with the same date of service and the same dollar amount
- Your patient’s plan has a non-standard preauthorization list
- You aren’t “in network” for the member