Health Alliance FLASH: Important COVID-19 Updates
March 24, 2020As the public health response to COVID-19 continues to progress, Health Alliance and Health Alliance Northwest will keep our providers informed of any related temporary changes in our policies, procedures and practices. Below are the most recent developments. Please note that these developments are in many cases temporary and subject to change in light of additional federal, state and industry directives and guidance.
Effective immediately, Health Alliance and Health Alliance Northwest are temporarily extending the claims timely filing requirement to 180 days. We recognize the demands being placed on our providers and their staffs during this extraordinary time, and we will continue to seek such actions that lessen our providers’ burdens.
Health Alliance and Health Alliance Northwest are temporarily broadening our telehealth codes to cover additional services, including behavioral health therapy, in response to the COVID-19 pandemic. This has been effective as of March 6 for our Medicare Advantage and Medicare Supplement plans, and as of March 19 for our fully-insured commercial plans, and will continue for the duration of the COVID-19 public health emergency. All appropriate telehealth services should be coded by the procedure code (CPT or HCPCS), with a Place of Service Code 02 (Telehealth), AND modifier -95, -GQ or -GT. We will now temporarily accept the following additional telehealth codes from authorized providers:
90791*, 90792*, 90832*, 90833*, 90834*, 90836*, 90837*, 90838*, 90847*, 98966, 98967, 98968, 98970, 98971, 98972, 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213*, 99214*, 99215*, 99421, 99422, 99423, 99441, 99442, 99443, G0406, G0407, G0408, G0425, G0426, G0427, G2010, G2012, G2061, G2062, G2063
Please note: all the above codes are temporarily covered unless otherwise specified in your provider agreement.
* Providers submitting claims for telehealth services using these codes must append with modifier 95.
In addition to expanding coverage to additional services, we will also temporarily cover the
full cost or waive in-network requirements for members on some of our plans. ** We recognize the advantages of telehealth services during this unique time, as they let members access certain types of care without having to visit the hospital or doctor’s office, where there might be greater risk of contracting COVID-19.
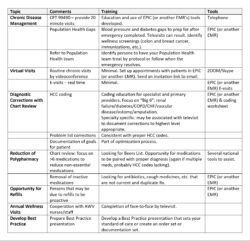
Finally, we also recognize that certain types of providers might begin to experience a prolonged period of time where their regular patients are asked to stay at home and avoid elective and/or less time-sensitive appointments. For such providers who find themselves with available time, we recommend activating value-driven activities that will help improve patient care and HCC coding. We have compiled a list, below, of value-driven activities that may be worth pursuing.
Provider Activities to Improve Care Value
As before, we invite our provider network to visit our COVID-19 webpage for up-to-date information about the illness, our response and questions about coverage. Thank you for your care, concern and selfless service for our members during this public health emergency.
** For Illinois fully-insured, Short-Term, Federal Employees Health Benefits (FEHB), State of
Illinois Active and State of Illinois MAPD plans: we are temporarily offering telehealth visits with
in-network providers at no cost to our members. For Medicare Advantage and Medicare
Supplement plans: members can temporarily see providers via telehealth at in-network cost sharing
levels, whether the provider is in their network or not. For Medicare Advantage this is an expanded
list offered under the temporary guidance that has been added to the already covered telehealth
codes. For Washington and Iowa fully-insured plans: we are temporarily covering the expanded
telehealth services with cost sharing for in-network services. Please note that IRS guidelines require
the application of a deductible for HSA-eligible high deductible health plans. Coverage specifics
for self-funded plans vary by employer. If members have any questions about coverage, you can
direct them to call the number on the back of their member ID card.