October Newsletter
October 10, 2014ICD-10 Update
The Department of Health and Human Services (HHS) officially pushed ICD-10 implementation back another year. According to an HHS press release, “This deadline allows providers, insurance companies and others in the healthcare industry time to ramp up their operations to ensure their systems and business processes are ready to go on Oct. 1, 2015.”
To learn more about the transition to ICD-10 or risk adjustment, visit us at CodingCounts.com or schedule a meeting with our coding consultant team.
Pharmacy Updates
Medicare
Medicaid (MMAI & SPD)
Formulary Additions
- Cyramza (ramucirumab)
- MMAI – Tier 2 with Preauthorization (PA)
- SPD – Covered with PA
- Dalvance (dalbavancin HCl)
- MMAI – Tier 2
- SPD – Covered with PA
- Sivextro (tedizolid phosphate)
- MMAI – Tier 2 with Quantity Limit of 6 doses in 30 days
- SPD – Covered with PA
- Gattex [teduglutide (rDNA origin)]
- MMAI – Tier 2 with PA
- SPD – Covered with PA
- Grastek (Timothy grass pollen allergen extract)
- MMAI – Tier 2
- SPD – Covered with PA
- Oralair (Sweet Vernal, Orchard, Perennial Rye, Timothy, and Kentucky Bluegrass mixed pollen allergen extracts)
- MMAI – Tier 2
- SPD – Covered with PA
- Ragwitek (short ragweed pollen allergen extract)
- MMAI – Tier 2
- SPD – Covered with PA
- Myalept (metreleptin)
- MMAI – Tier 2 with PA
- SPD – Covered with PA
- Otezla (apremilast)
- MMAI – Tier 2 with PA
- SPD – Covered with PA
- Sylvant (siltuximab)
- MMAI – Tier 2 with PA
- SPD – Covered with PA
- Tretten [Coagulation Factor XIII A-Subunit (Recombinant)]
- MMAI – Covered under Part B
- SPD – Covered with PA
- Zykadia (ceritinib)
- MMAI – Tier 2 with PA
- SPD – Covered with PA
Revised Policy
- Lansoprazole Step-Edit – Coverage of lansoprazole requires documentation of previous trial and subsequent failure or intolerance of or contraindication to omeprazole and pantoprazole
Commercial
Formulary Additions
- Entyvio (vedolizumab)
- Tier 5 with PA
- Jublia (efinaconazole
- Tier 3 with PA
- Cyramza (ramucirumab)
- Tier 5 with PA
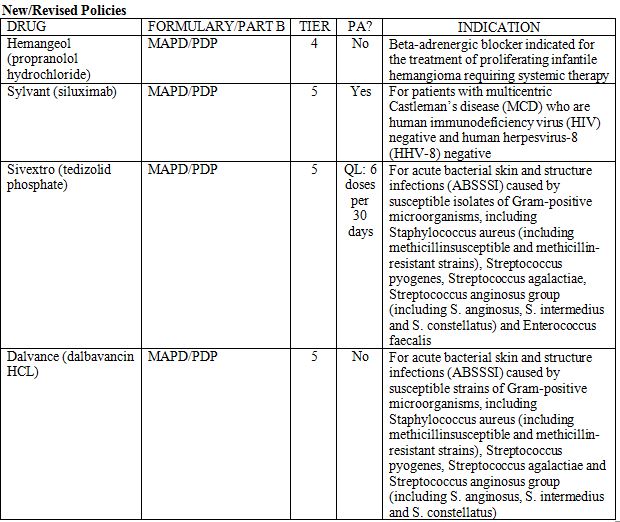
- Sylvant (siluximab)
- Tier 5 with PA
- Grastek (Timothy grass pollen allergen extract)
- Tier 3
- Zontivity (vorapaxar sulfate)
- Tier 3 with Step-Edit
- Sivextro (tedizolid phosphate)
- Tier 5 with Quantity Limit of 6 doses per 30 days
- Dalvance (dalbavancin HCL)
- Tier 5
- Kadcyla (trastuzumab emtansine)
- Tier 5 with PA
Revised Policies
- Matulane
- PA now required (also moved from Tier 2 to Tier 5 Specialty Pharmacy)
- Lotronex
- PA now required
- Advair
- PA now required for all strengths and indications (new starts only)
- Flovent
- PA now required (new starts only)
- Diabetes Drug Therapies
- Removed HbA1c requirements, Byetta and Bydureon Step-Edit through Victoza, and SLGT-2 Step-Edit through DPP-4
- Added Nesina, Oseni, and Kazano to DPP-4 section
- Changed approval period to one year
Formulary Changes
- Moved from Tier 2 to Tier 3
- Advair
- Flovent
- Victoza
- Moved from Tier 3 to Tier 2
- Aerospan
- Asmanex
- Pulmicort
- Dulera
- Brilinta
- Lumigan
- Restasis
- Grastek
- Ragwitek
DEA Ruling on Hydrocodone Combination Products
The Drug Enforcement Administration (DEA) has ruled to move hydrocodone combination products (HCPs) from Schedule III to Schedule II. This change went into effect on October 6, 2014.
The DEA’s regulations and recommendations include:
- Use electronic health records systems to help identify patients currently receiving chronic hydrocodone combination drugs. Discuss alternative pain management options.
- Refills will be valid only if the original prescription was written before October 6 and is filled before April 8, 2015. Certain pharmacy dispensing software products will be unable to process existing refills starting on October 6, so prescribers should be prepared to work with pharmacists to supply new scripts when necessary.
- Prescriptions for HCPs issued on October 6 or later must comply with Schedule II regulations, which include no refills and no over-the-phone or fax submissions (except in rare situations). Electronic transmission of prescriptions is valid only if legal in the prescriber’s state.
- If appropriate and allowed by a prescriber’s state, the prescriber can write multiple HCP prescriptions to provide a 90-day supply and indicate the earliest fill date on each prescription.
Medicaid Updates & Reminders
- As of August 25, 2014, Health Alliance Connect preauthorizations (both inpatient and outpatient services) were transitioned to the Health Alliance Quality and Medical Management staff. All medical preauthorizations for all plan types are now being processed by the Medical Management Department in Urbana. The preauthorization fax number for Health Alliance Connect has been redirected to the Health Alliance fax number, 217-337-8440, and authorization requests submitted via Clear Coverage are also being worked through this same process. For events before August 25, contact Health Alliance Connect, which is working any open events.If you have any questions or need help for preauthorizations after August 25, email these staff members in Medical Management:
- Inpatient: Ellen.Cruchelow@healthalliance.org
- Outpatient: Kathy.Hershberger@healthalliance.org
- Medicaid prescriptions for eyeglasses can be sent directly to JAK Lab. JAK Lab is able to produce the eyeglasses within 30 days. You do not need to go through Health Alliance Connect for approval before sending to JAK Lab.
- Send Illinois Partnership for Health member claims directly to Illinois Department of Healthcare and Family Services, not to Health Alliance Connect. We also do not handle inpatient reviews or any utilization management, such as preauthorization. These reviews and preauthorization continue to be handled by Illinois Department of Healthcare and Family Services.
- Spinal manipulations and chiropractor visits are not on the preauthorization list for the Medicaid population (SPD, DUA, FHP), so we will not be reviewing for these services. The service should be covered up to 12 visits per year for the SPD/ICP, MMAI, and FHP population with a contracted provider. If the member needs more visits, it will need to be submitted for a medical necessity review. ICP/MMP members do not have a limit on visits as long as they use a contracted provider. For the FHP and ACA population, spinal manipulations and chiropractor visits are only covered for members under 21.
Send us Secondary Claims Electronically
Did you know that we can accept secondary claims electronically? We just need the primary insurance information (paid amount, member responsibility, and adjusted amount) to be included on the 837 (electronic form), and your secondary claim can be processed without you having to take the time and effort to drop it to paper and send us a paper copy of the primary EOB. This will save your office time, and it will help speed up claims processing. Contact your provider relations specialist if you have any questions about submitting your secondary claims electronically.
New Preauthorization Software Coming
Novologix (owned by CVS Caremark) is a pharmacy software system with 2 main functions, automated claims processing for drugs dispensed on the medical side and a provider Web portal for drug preauthorizations. Only the preauthorization function will affect you.
We will start using Novologix in December, but we will not require providers to request preauthorization through the new program until next year. We will update you with more information as that transition date approaches. CVS Caremark will also offer online training and Q&A sessions to help you learn how to access its website, request preauthorization, and review the status of authorized services.
Improving our HEDIS® Scores for Retinal Eye Exams
The percentage of members with diabetes who receive a retinal eye exam is one of the measures we report as part of the annual HEDIS audit. HEDIS specifications require people with diabetes to get a retinal or dilated eye exam every year or every other year if the previous exam shows no retinopathy. An eye care professional must perform the exam.
For the last several years, our plans have scored just above the NCQA Quality Compass® National Average in this measure. These are the 2014 HEDIS scores:
- Commercial HMO/POS – 61%
- Commercial PPO – 50%
- Medicare Advantage HMO – 70%
- Medicare Advantage PPO – 68%
The commercial PPO plan shows a decline from 56% reported in 2013. The other plans remained unchanged.
We want to improve these scores in all 4 categories as we strive to achieve HEDIS scores at the Quality Compass 90th percentile level. For the commercial HMO/POS, that would be 725, and for the commercial PPO plans, that would be 615. Medicare Advantage Quality Compass National Averages have not been released for 2014.
Note:
- Most Health Alliance plans cover retinal eye exams as a medical benefit for members with diabetes.
- Primary care physicians should discuss the need for retinal eye exams with their patients who have diabetes.
- Eye care providers can help improve HEDIS rates and ensure their patients with diabetes receive recommended care by following these guidelines:
- Ask all patients if they have diabetes, and if so, clearly document it in the medical record.
- Perform a retinal or dilated eye exam annually or every other year if no retinopathy.
- Clearly document findings in the medical record.
- Submit the claim to us, indicating the diagnosis.
- For questions, contact Reba Karr at Reba.Karr@healthalliance.org or 217-337-8074.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). Quality Compass® is a registered trademark of the National Committee for Quality Assurance (NCQA).
Remind Patients to Get Flu Vaccine
With flu season approaching, remind your patients, our members, to protect themselves and those around them with a flu shot. Most of our plans cover 100% of the shot when using an in-network provider or any pharmacy.
Members can check their coverage on Your Health Alliance or call the number on the back of their member ID card.
Help Improve our Health Outcomes Survey Scores
One way that Centers for Medicare & Medicaid measures quality of care provided by Medicare Advantage plans is through the Health Outcomes Survey (HOS). In collaboration with the National Committee for Quality Assurance, a random sample of our Medicare Advantage members are surveyed to measure and assess physical and mental functioning over time.
Even though HOS involves member-reported information, it is important for you to keep discussing these areas with your patients:
- Improving Bladder Control – In 2014, the Medicare Advantage HMO plan scored 33%, and PPO scored 35% for the HEDIS Measure of Improving Bladder Control, which means only about one-third of those members who reported having urinary incontinence received treatment. According to the Agency for Healthcare Research and Quality, urinary incontinence may cause a wide range of problems, including cellulitis, pressure ulcers, urinary tract infections, falls with fractures, sleep deprivation, social withdrawal, depression, and sexual dysfunction.
- How can you help? Ask questions and educate members on treatment options for improving bladder control.
- Reducing Risk of Falling – HOS asks members if they have fallen or had problems with balance in the past 12 months. If they answer yes, the survey then asks if their doctor suggested intervention to decrease fall risk. The Medicare Advantage PPO scored 55%, which is a 1% decrease from last year, and the HMO plan scored 62%, which is a 2% decrease from last year. Falling can cause hip fractures and head trauma and can even increase risk of early death.
- How can you help? During office visits, ask patients about problems with balance or recent falls, and recommend a walker or cane if needed.
- Monitoring Physical Activity – The survey asks members if their doctor advised them to start, decrease or maintain their level of physical activity. The PPO rate for recommending activity was 46%, which is 2% less than last year. The HMO plan was 44%, which is a 4% decrease from last year. Older adults can benefit greatly from muscle-strengthening activities. Stronger muscles help reduce the risk of falling and improve the ability to perform the routine tasks of daily life.
- How can you help? Discuss activity levels with Medicare Advantage members, including the SilverSneakers® fitness program, which is available to them for no additional cost. Members can learn more at SilverSneakers.com or by calling 1-888-423-4632.If you have questions about SilverSneakers, call Health Alliance Wellness Administrator Karen Stefaniak at 217-383-8197 or email Karen.Stefaniak@healthalliance.org.
2014 Health Alliance Coding Workshop
Join us as we discuss the advancements in health insurance and how these changes affect you.
When: Thursday, October 23, 2014 from 6-8 p.m. Doors open at 5:30 p.m. for hors d’oeuvres and refreshments.
Where: The Forum at Carle Foundation Hospital
Topics include:
- Risk adjustment overview
- Strategies for success with diabetic patients
- Understanding our risk adjustment efforts
- Open forum Q&A session
The seminar is open to all healthcare professionals who provide care, document services, code, or bill in any of our participating provider groups and offices. Approved for 2.0 AMA PRA Category 1 CreditsTM.
By the end of the seminar, you’ll be able to:
- Define risk adjustment and the patient populations it involves
- Develop quality strategies for diabetic patients
- Understand the efforts of oue risk adjustment team
Seats are limited. RSVP to CodingCounts@healthalliance.org by Thursday, October 16.

Carle Foundation Hospital is accredited by the Illinois State Medical Society to provide continuing medical education for physicians.
Carle Foundation Hospital designates this live activity for a maximum of 2.0 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Remind Patients about Colorectal Cancer Screenings
Early detection is key for the prevention and treatment of colorectal cancer. But about 1 in 3 U.S. adults age 50-75 have not been tested for colorectal cancer, according to a 2013 report from the Centers for Disease Control and Prevention. That’s about 20 million people who should get tested but haven’t.*
Help make sure your patients, our members, don’t fall into that category. Talk with your patients ages 50-75 about their screening options. Most of our plans cover 100% of a fecal occult blood testing, colonoscopy, or sigmoidoscopy.*
*As recommended by the United States Preventive Services Task Force
**If they need any more testing or related services, copay/coinsurance may apply.
Check BMI Annually
Remember to measure height and weight to calculate BMI for all patients, adults and children, at least once a year. This simple test can help raise awareness for those who show a gradual increase in BMI. It also can help direct treatment, exercise, and nutrition changes for those already in the overweight or obese range.
HEDIS requires Health Alliance to verify documentation in the medical record, noting BMI value for adults and BMI percentile for children. Weight and height should also be clearly documented annually in the medical record.
Helping patients understand what their BMI range should be and how to get there can start them on a path to better health and can improve our HEDIS measures during medical record audits.
Weight is a sensitive topic, but recording BMI measurements is important. Remember to calculate and document each patient’s BMI at least once a year, and talk to your patients about any concerns you have based on their results.
Help Your Patients Make the Most of Their Golden Years
Please tell your patients about our upcoming event, Aging Happily—Making the Most of Your Golden Years.
When: October 20, 5:30–7:30 p.m.
Where: Carle Foundation Forum – Pollard Auditorium, Urbana
What:
- Helpful info about improving emotional and mental health and staying active and socially connected
- Q&A with speakers
- Info booths
Guests will enjoy free parking and free snacks. Those interested should RSVP by October 15 to Danielle Daly at 1-800-851-3379, ext. 4643.