Reid April Newsletter 2021
April 20, 2021A Message of Continued Gratitude
It’s now been over a year since COVID-19 first emerged in our country and began its spread through our communities. Acknowledging this grim and solemn milestone, we wanted to express our immense gratitude for all you’ve done for our members this past year. You’ve taken care of the physical and mental health of individuals, families and entire communities, sacrificing of yourself to be there for others. We know the pandemic continues and difficult months still lie ahead, but thanks to your constant care and vigilance we’re headed in the right direction, with renewed optimism and strength. Thanks for being that shining light, that healing hand, that source of hope. From all of us – and our members – the deepest gratitude.
Care Coordination and Health Coaching:
Tell Your Patients About These Free Services
Together we can help your patients meet their health goals. We offer free care coordination and health coaching to all your patients who have us as their insurance. These services pair them with our highly skilled nurses, social workers and health coaches, who offer a variety of support between visits to your office.
Our care coordinators and health coaching teams can assist your patients with setting and reaching health and wellness goals. Not only do we help them find great tools and resources to keep them healthy, but we provide tangible, needed support – we help them understand and manage illness and recovery, coordinate their care when they have complicated health conditions and assist them in caring for themselves to help prevent illness and hospital stays.
Our care coordination and health coaching can assist with any disease state or condition – for example: CHF, COPD, diabetes, high blood pressure, behavioral health issues, high-risk pregnancies, NICU stays for newborn babies, oncology, transplant services and more. Our health coaches focus on lifestyle changes for your patients, in general or to help with new diagnoses such as diabetes or high blood pressure. They provide coaching and education about managing healthy lifestyles and improving well-being. Our teams work in collaboration with your patients to help them meet their goals.
To refer a patient or get more information, please call us at (800) 851-3379, ext. 28947, or email us at Care.Coordination@healthalliance.org. Thanks for all you do for our members’ health and well-being.
We’ve Expanded Our Substitution Code List
We’re happy to announce that we’ve expanded our Substitution Code List. We’ve added over 4,500 substitutable CPT and HCPCS codes to our claims process to help with quick and accurate claims payment while removing roadblocks for you and your staff.
We created the Substitution Code Crosswalk Table to help you easily determine when the claim will pay correctly. You’ll be able to find this Crosswalk Table by logging in to your account on Provider.HealthAlliance.org. You read the table from left to right. Below are some example scenarios.
Scenario A:
- You obtain a prior authorization for code 19368, but code 19350 is performed: claim will pay.
Scenario B:
- No prior authorization is needed for code 11440, but code 11446 is performed: claim will pay.
Scenario C:
- You obtain a prior authorization for code 73202, but code 73218 is performed: the claim will not pay. You’ll have 7 days from the date of service to contact us or eviCore to have the additional codes or substitution codes reviewed. If the request is not made within that timeframe, or if the criteria is not met, the charges will not be covered.
Scenario D:
- No prior authorization is needed for code 63688, but code 63685 is performed: the claim will not pay. You’ll have 7 days from the date of service to contact us or eviCore to have the additional codes or substitution codes reviewed. If the request is not made within that timeframe, or if the criteria is not met, the charges will not be covered.
We’re very happy to bring you this expansion of our Substitution Code List and this helpful crosswalk tool. If you have any questions whatsoever, or need help finding or understanding the Crosswalk Table, please contact your provider relations specialist at (800) 851-3379 or email us at provider.relations@healthalliance.org. You can also contact eviCore at (855) 252-1117. Thank you.
Help Us Move the Needle
Care for Patients With Hypertension
Hypertension is the most common reason people visit a clinician. It affects almost one-third of American adults and is uncontrolled in nearly half of the cases. Hypertension is not only common, but dangerous too – it’s a major risk factor for heart disease, stroke and kidney disease. In fact, for individuals age 40 to 89, the risk of death from ischemic heart disease and stroke doubles for every 20 mm Hg. With hypertension both so common and so harmful, here are some important tips for you and your staff:
- Consider further clinical intervention for your patients with uncontrolled hypertension.
- Provide both initial and ongoing training to your staff to make sure they’re taking blood pressure readings correctly. This includes these practices:
- Have patients sit in a chair with their feet on the floor and their arm supported so their elbow is at heart level. The inflatable part of the cuff should completely cover at least 80% of the upper arm. The cuff should be placed on bare skin, not over a shirt, and make sure to have the patient remove any tight-sleeved clothing.
- Encourage staff to assess whether patients have used nicotine or caffeine, have exercised in the last 30 minutes or have a full bladder, since these can affect the reading.
- When blood pressure shows up as elevated, take a second reading after the patient has rested.
- Encourage your patients to monitor their blood pressure at home, and don’t forget to ask patients to bring their home blood pressure cuff into your office for calibration.
Note: With the expanded use of telehealth, NCQA has made changes allowing increased inclusion criteria for blood pressure monitoring, to now also include member-reported blood pressures taken on any remote digital device for the Controlling Blood Pressure HEDIS® measure. The patient-reported blood pressure must be recorded and dated in the patient’s chart. Patient-reported blood pressures taken with a manual cuff are not acceptable. See this CDC webpage for more information. - Educate your patients on their blood pressure goals, as well as when to report their at-home readings.
- Encourage patients to lead a healthier lifestyle, including maintaining a healthy weight, reducing sodium intake and getting enough exercise.
- Stress the importance of medication adherence to your patients.
- Consider prescribing a statin medication as well.
- Consider non-pharmacological treatments in addition to medications.
- Encourage patients to sign up for health coaching or care coordination. Our members can call the number on the back of their Member ID card to learn more.
Improve Medication Adherence
For those with diabetes, hypertension and hypercholesterolemia, there’s a correlation between medical adherence and reductions in complications and hospitalizations. Unfortunately, only about half of U.S. patients take their medicines as directed by their doctor. We all can help change this. Here are some suggestions:
- Write 90-day prescriptions. Fewer refills means fewer opportunities for your patients to forget picking them up.
- Synchronize refills of chronic medications. This lets patients pick up multiple refills at the same time.
- Encourage your patients to call the number on the back of their insurance ID card to see if they can save money through prescription mail order.
- Prescribe generic medications when appropriate.
- Make sure your patients understand why they’re taking the medication and the importance of taking it consistently. Give patients the materials they need to understand their chronic disease and the medication they’re prescribed.
- Encourage patients to get their Comprehensive Medication Review. In addition, encourage those who qualify to also complete their Medication Therapy Management.
- Assess for patient barriers to taking their medications as directed, such as concerns about side effects, costs, transportation issues or knowledge deficits about their chronic disease or the purpose for their medications.
- Make sure patients know what to do if they miss a dose.
- Educate patients about any side effects that can be avoided by taking a medication with food or at a different time of the day. Make sure patients know whether to take their medications on a full or empty stomach.
- Encourage patients to reach out to health coaches and/or care coordinators, who can help them stick to their routine. Our members can call the number on the back of their Member ID card to learn more.
- Advise patients to tie taking their medications with a daily routine, such as brushing their teeth. This helps them remember to take them every day.
- Have patients keep a medication log or calendar that records when they take each dose.
- Advise your patients to always bring enough medication when traveling, and to bring a few extra days’ worth in case their travel is prolonged or delayed. If flying, they should keep their medication in a carry-on bag for easy access.
Medicines only work if people take them. Give your patients the knowledge, help and support they need to stick to their medication plans. Thank you, as always, for your dedication and support to our members.
The “Big Six” – Diabetes without Complications
Supporting documentation and accurate coding are key to making sure your patients get the care they need. Failure to document chronic conditions on an annual basis impacts your patients (our members), fellow providers and our organization. Here’s some helpful information about coding for Diabetes without Complications, one of the “Big Six” diagnosis categories most frequently miscoded or unsupported in documentation.
All diabetes mellitus code sets include a “without complication” designation. Diabetes mellitus without complications should only be reported when there is no causal relationship between diabetes and another condition, such as chronic kidney disease, neuropathy, circulatory disease or something else.
When a condition could be caused by or related to a patient’s diabetes but is not, documentation needs to clearly state that the conditions are unrelated or due to an underlying cause besides the patient’s diabetes mellitus.
For example: “Patient has Type 2 diabetes managed by insulin. Polyneuropathy due to chemo has recently worsened – will start Gabapentin.” In this scenario, it’s clear the polyneuropathy is unrelated to the diabetes – therefore, reporting both E11.9 Type 2 diabetes mellitus without complications and G62.0 Drug induced polyneuropathy would be appropriate, instead of reporting E11.42 Type 2 diabetes mellitus with diabetic polyneuropathy.
Here are the various codes for diabetes mellitus without complications:
|
Code |
Description |
|
E08.9 |
Diabetes mellitus due to underlying condition without complications |
|
E09.9 |
Drug or chemical induced diabetes mellitus without complications |
|
E10.9 |
Type 1 diabetes mellitus without complications |
|
E11.9 |
Type 2 diabetes mellitus without complications |
|
E13.9 |
Other specified diabetes mellitus without complications |
Finally, remember to use at least one component of M.E.A.T. to support the diagnosis you’re reporting:
- Monitor: disease progression/regression, symptoms and give a status.
- Evaluate: review test results, medication or treatment effectiveness.
- Assess: counsel, order tests, review records.
- Treat: medications, therapies, referrals.
Thank you for your constant care and dedication to our members’ health.
Learn More About Asthma Care
If you or your staff want to learn more about asthma care, there’s a great resource we can point you to. The American Lung Association’s Asthma Basics program is offered as a self-paced online learning module or an in-person workshop. The program is ideal for frontline healthcare professionals, such as school nurses or community health workers, as well as individuals with asthma, parents of children with asthma, and co-workers, friends and family who want to learn more about the condition. The Asthma Basics online learning module is available in English and Spanish.
This program teaches participants to:
- Recognize and manage triggers.
- Understand the value of an asthma action plan.
- Recognize and respond to a breathing emergency.
- And much more.
One of the highlights of the program is an animation that shows the three primary changes in the airways during an asthma episode.
Asthma Basics also includes comprehensive resources, including asthma medication devices, demonstration videos and downloads.
If you have any questions about registering for the online course, visit Online Learning Course Support to see potential solutions or to request more help. To learn more about how to host an Asthma Basics in-person workshop, please contact your local American Lung Association office.
Remind Your Patients:
Get Screened for Colorectal Cancer
According to American Family Physician, colorectal cancer is the second leading cause of cancer death in the U.S – but because it often takes time to develop, the disease can be detected early when treatment is most successful. That’s why regular colorectal cancer screenings are so important.
The American College of Physicians recommends routine screenings for all average-risk adults age 50 – 75. Multiple screening types are available, with choice based on a patient’s health condition, the doctor’s judgment and patient preference.
- FIT (fecal immunochemical test), annually.
- Cologuard®, every three years.
- Flexible sigmoidoscopy, every five years.
- Colonoscopy, every 10 years.
Whichever test your patient chooses, we cover it at 100%. If additional testing or related services are needed, copay may apply. To check for exact coverage, your patients should call the customer service number on the back of their insurance ID card.
Don’t Forget Chlamydia Screenings
American Family Physician also reminds us of the importance of chlamydia screenings. The U.S. Preventive Services Task Force recommends routine screening for all sexually active women age 24 and younger, and for those 25 and older at increased risk due to having a new partner or multiple partners. All pregnant women at increased risk should be screened for chlamydia during their first prenatal visit, due to the high risk of intrauterine and postnatal complications if left untreated. Also, any pregnant woman terminating their pregnancy should be screened. Currently, there isn’t sufficient evidence to recommend chlamydia screening in men, although a small number of studies suggest screening high-risk groups may be both useful and cost-effective.
Improving Screening for Patients with Metabolic Syndrome Who Take Antipsychotic Medications
Metabolic syndrome includes several features – among them, glucose intolerance/insulin resistance, hypertension, obesity and dyslipidemia. These features often result in cardiovascular disease and type 2 diabetes. Seriously mentally ill patients who are diagnosed with psychotic disorders often receive antipsychotic medications, and this population is also at high risk for metabolic syndrome. Even without the antipsychotic medications, this population is at high risk.
Unfortunately for this at-risk population, the screening rates for metabolic syndrome are currently below the recommended rates. There’s a continued need to increase these screenings so they can get the help they need for their health and well-being. Baseline measures (for the purposes of monitoring) should be obtained before starting an antipsychotic regimen for these patients, and they should include:
- Height and weight.
- BMI calculation.
- Waist circumference.
- Personal and family history of:
- Diabetes.
- Dyslipidemia.
- Hypertension.
- Obesity.
- Cardiovascular disease.
- Blood pressure.
- Fasting plasma glucose.
- Fasting lipid profile.
In addition, there should be ongoing monitoring of the following:
- Metabolic risk consideration when initiating second generation antipsychotic medication.
- Regular monitoring against the baseline screening for metabolic syndrome.
- Education to patient, family and caregivers.
- Referrals to specialists when appropriate.
- Consideration of medication changes if deemed necessary.
Thank you for your dedication, attention to detail, and support for the physical and mental health of all our members. We deeply appreciate all you do.
HPV Vaccination Rates High at Carle Urbana on Windsor
As you may know, HPV vaccination rates are universally low. Therefore, we’re encouraged that a major pediatrics clinic in our provider network, Carle Pediatrics (at Carle Urbana on Windsor, in Urbana, IL), has an HPV vaccination rate of 68.5% for 13 – 17 year-olds. In comparison, only 54% of teens nationwide and 55% of teens in Illinois, 41% in Indiana, 61% in Iowa and 53% in Washington are up to date on all the recommended doses of the HPV vaccine, according to the Centers for Disease Control and Prevention (CDC).
The CDC recommends 11 – 12 year-olds, both girls and boys, get two doses of the HPV vaccine to prevent HPV-caused cancers.
The CDC suggests you take action by:
- Knowing your state and region’s HPV vaccine coverage rates to see how you’re doing with HPV vaccination in comparison to others.
- Sharing information about your state and region’s HPV vaccination rates with your office staff and colleagues.
- Identifying ways you can boost HPV vaccination rates in your practice, and sharing what’s working in your practice with other providers in your community and region. Together we can all encourage and help one another boost rates.
Please help protect your young patients by urging parents to vaccinate their children against HPV. And thanks for all you’re already doing in this and other efforts to help our members get the preventive care they need. As a final note, please make use of these two helpful resources from the CDC:
- HPV vaccine schedule and dosing information.
- Full immunization schedule – listing all recommended vaccines – for children, adolescents and teens (birth to age 18).
Pharmacotherapy for Schizophrenia and Bipolar Disorders
In general, there’s a high rate of non-adherence to antipsychotics in the treatment of schizophrenia and bipolar disorders. This non-adherence is often due to denial of the illness, downplaying of the severity of the illness or negative attitudes about medications. Whatever the reason, non-adherence can lead to many problems. For example, there’s greater chance of relapse, which results in repeated inpatient admissions and emergency department visits. An increase in mood episodes and suicide attempts are also associated with non-adherence.
Long-acting injectable antipsychotic drugs are an option for many of those who may otherwise not adhere to their antipsychotic treatment regimen. These medications are often administered with two- or four-week intervals and include:
- Aripiprazole (extended release or lauroxil).
- Fluphenazine decanoate.
- Haloperidol decanoate.
- Olanzapine pamoate.
- Paliperidone palmitate (4- or 12-week).
- Risperidone (extended SQ or microspheres).
Use of long-acting injectables is suggested for those patients who have proven to be non-adherent with their oral medications. Administering a long-acting injectable can also be considered for those in this population who:
- May benefit form consistent blood levels of medications.
- Prefer the injectable.
- Have concurrent substance use disorders and are non-adherent with antipsychotic oral medications.
- May have poor absorption with oral medications (often due to general malabsorption issues or intestinal bypass, for example).
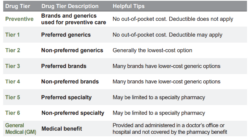
Pharmacy 101: What are Tier Levels on Formularies?
We know formularies can be confusing. To help answer common questions and help you and your staff understand more about our pharmacy coverage, we’re beginning a series of “Pharmacy 101” articles. This month we’ll discuss tier levels, and stay tuned each issue as we tackle new subjects.
On a formulary, medications are listed by categories or classes, and they’re placed into levels called tiers. Tiers are simply the different cost levels that members will pay for a medication. Generally, the higher the medication’s tier, the more a member will pay out of pocket for it. Prescribing a lower tier or preferred medication can help a member pay the lowest out-of-pocket cost.
A plan may have multiple or no tiers. Below is an example of what a typical commercial plan may have outlined for its medication formulary and tier levels. Please note: the tier structure of each plan varies depending upon the elected benefits, which are outlined in the Summary of Benefits document provided to each member. Also note, different plans may have different member costs (copays/coinsurance) associated with these tiers. For instance, instead of having no out-of-pocket costs like the example shown below, a different plan’s Tier 1 may have a copay. Finally, please note: if a member has a high-deductible plan, the tier cost levels will apply once the member has met their deductible.
On Medicare plans, the cost of medications is also dictated by the tier structure, and this is set by the Centers for Medicare & Medicaid Services (CMS). The standard pharmacy benefit for 2021 is as follows:
Deductible: $0
Tier 1: $2 copay
Tier 2: $15 copay
Tier 3: $47 copay
Tier 4: 50% coinsurance
Tier 5: 33% coinsurance
Once a member has received pharmacy benefits totaling $4,130, the member will then be in the “donut hole.” At this time, the member pays 25% for all drugs until true out-of-pocket (TROOP) costs reaches $6,550. The member will then be in the catastrophic phase and copays will be significantly less.
All our formularies are accessible online at HealthAlliance.org. There’s also a very helpful Provider Resources page on our website that includes prior authorization forms, tools and guides, and a pharmacy section that includes the formularies, forms, Medicare information and a section for codes.
If you have any questions whatsoever, please contact your provider relations specialist at (800) 851-3379 or email us at provider.relations@healthalliance.org. We’re always happy to help!
Pharmacy Updates
Medicare
Oncology/Hematology
Formulary Additions
- Ayvakit (avapritinib)—Treatment of unresectable or metastatic gastrointestinal stromal tumor harboring a PDGFRA exon 18 mutation, including PDGFRA D842V mutations in adults
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Blenrep (belantamab mafodotin)—Treatment of relapsed or refractory multiple myeloma in adults who have received at least 4 prior therapies, including an anti-CD38 monoclonal antibody, a proteasome inhibitor, and an immunomodulatory agent
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Danyelza (naxitamab)—Treatment of relapsed or refractory high-risk neuroblastoma in the bone or bone marrow (in combination with granulocytemacrophage colony-stimulating factor [GM-CSF]), in pediatric patients ≥1 year of age and adults who have demonstrated a partial response, minor response, or stable disease to prior therapy
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Gavreto (pralsetinib)—Treatment of metastatic RET fusion-positive nonsmall cell lung cancer (NSCLC) in adults as detected by an approved test. Treatment of advanced or metastatic RET fusion-positive thyroid cancer in pediatric patients 12 years of age or older and adults who require systemic therapy and who are radioactive iodine-refractory (if radioactive iodine is appropriate). Treatment of advanced or metastatic RET-mutant medullary thyroid cancer in pediatric patients 12 years of age or older and adults who require systemic therapy
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Inqovi (decitabine and cedazuridine)—Treatment of myelodysplastic syndromes (MDS), including previously treated and untreated, de novo and secondary MDS with the following French-American-British subtypes (refractory anemia, refractory anemia with ringed sideroblasts, refractory anemia with excess blasts, and chronic myelomonocytic leukemia [CMML]) and intermediate-1, intermediate-2, and high-risk International Prognostic Scoring System groups, in adults
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Jelmyto (mytomycin) ureteral gel—Treatment of low-grade upper tract urothelial cancer in adults
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Monjuvi (tafasitamab)—Treatment (in combination with lenalidomide) of relapsed or refractory diffuse large Bcell lymphoma (DLBCL) not otherwise specified in adults, including DLBCL arising from low grade lymphoma, and who are not eligible for autologous stem cell transplant
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Onureg (azacitidine)—Treatment of acute myeloid leukemia in adults who achieved first complete remission (CR) or complete remission with incomplete blood count recovery (Cri) following intensive induction chemotherapy and are not able to complete intensive curative therapy
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Orgovyx (relugolix)—Treatment of advanced prostate cancer
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Pemazyre (pemigatinib)—Treatment of previously treated, unresectable locally advanced or metastatic cholangiocarcinoma in adults with a fibroblast growth factor receptor 2 fusion or other rearrangement (as detected by an approved test)
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Phesgo (pertuzumab, trastuzumab, and hyaluronidase)—Neoadjuvant treatment of HER2-positive, locally dvanced, inflammatory, or early stage breast cancer (either > 2 cm in diameter or node positive), in combination with chemotherapy, as part of a complete treatment regimen for early breast cancer in adults; adjuvant treatment of HER2-positive early breast cancer, in combination with chemotherapy, in adults at high risk of recurrence. Treatment of HER2-positive metatatic breast cancer (incombination with docetaxel) in adults who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Qinlock (ripretinib)—Treatment of advanced gastrointestinal stromal tumor (GIST) in adults who have previously received treatment with ≥3 kinase inhibitors, including imatinib
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Retevmo (selpercatinib)—Treatment of metastatic RET fusion-positive non-small cell lung cancer (NSCLC) in adults. Treatment of advanced or metasttic RET-mutant medullary thyroid cancer (MTC) in adults and pediatric patients 12 years of age and older who require systemic therapy. Treatment of advanced or metastatic RET fusion-positive thyroid cancer in adults and pediatric patients 12 years of age and older who require systemic therapy and who are refractory to radioactive iodine (if radioactive iodine is appropriate)
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Sarclisa (isatuximab)—Treatment of multiple myeloma (in combination with pomalidomide and dexamethasone) in adults who have received ≥2 prior therapies including lenalidomide and a proteasome inhibitor
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Tabrecta (capmatinib)—Treatment of metastatic non-small cell lung cancer (NSCLC) in adults whose tumors have a mutation that leads to mesenchymal-epithelial transition (MET) exon 14 skipping as detected by an approved test
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Tazverik (tazemetostat)—Treatment of metastatic or locally advanced epithelioid sarcoma not eligible for complete resection in adults and adolescents 16 years of age and older. Treatment of relapsed or refractory follicular lymphoma in adults whose tumors are positive for an EZH2 mutation (as detected by an approved test) and who have received at least 2 prior systemic therapies. Treatment of relapsed or refractory follicular lymphoma in adults who have no satisfactory alternative treatment options
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Tecartus (brexucabtagene autoleucel)—Treatment of relapsed or refractory mantle cell lymphoma (MCL) in adults
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Trodelvy (sacituzumab govitecan)—Treatment of metastatic triple-negative breast cancer in adults who have received ≥2 prior therapies for metastatic disease
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
- Tukysa (tucatinib)—Treatment of advanced unresectable or metastatic human epidermal growth factor receptor 2 (HER2)-positive breast cancer (in combination with trastuzumab and capecitabine) in adults with or without brain metastases who have received ≥1 prior anti-HER2-based regimens in the metastatic setting
- Formulary placement recommendations
- Medicare—Tier 5 with PA; Reviewed by Health Alliance
- Formulary placement recommendations
- Zepzelca (lurbinectedin)—Treatment of metastatic small cell lung cancer in adults with disease progression on or after platinum-based chemotherapy
- Formulary placement recommendations
- Medicare—Part B; Reviewed by eviCore
- Formulary placement recommendations
Criteria Changes
- Sandostatin (octreotide) and Sandostatin LAR (octreotide)
- Added criteria for Acute chemo related diarrhea and treatment of diarrhea associated with GVHD
New Policy
- Jakafi
- New indication for Graft versus Host Disease (GVHD) necessitated HA in-house PA criteria
Infectious Disease
Formulary Additions
- Fetroja (cefiderocol)—Treatment of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia, caused by the following susceptible gramnegative microorganisms: Acinetobacter baumannii complex, Escherichia coli, Enterobacter cloacae complex, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Serratia marcescens, in patients ≥18 years of age.
- Formulary placement recommendations
- Medicare—Tier 5
- Formulary placement recommendations
- Lampit (nifurtimox)—For use in pediatric patients from birth to less than 18 years of age that weigh at least 2.5kg for the treatment of Chagas disease (American Trypanosomiasis) caused by Trypanosoma cruzi. Chagas is an infectious tropical disease that affects an estimated 300,000 people in the US
- Formulary placement recommendations
- Medicare—Non-Formulary
- Formulary placement recommendations
- Rukobia (fostemsavir)—Treatment of HIV-1 infection, in combination with other antiretrovirals, in heavily treatment-experienced adults with multidrug-resistant HIV-1 infection failing their current antiretroviral regimen
- Formulary placement recommendations
- Medicare—Tier 5
- Formulary placement recommendations
Criteria Changes
- Dificid (fidaxomicin) Step-Edit
- Removing PA is appropriate given that Dificid is now a first-line therapy
- Hepatitis B Treatment – Hepsera, Baraclude, & Vemlidy
- Removed abstinence requirement following updated AASLD guidelines and feedback from Carle Addiction Recovery Center
- Hepatitis C Treatment
- Removed Olysio and Daklinza since they’re no longer on the market
- Specified that diagnosis must be chronic Hepatitis C infection
- Removed abstinence requirement following updated AASLD guidelines and feedback from Carle Addiction Recovery Center
- Will accept provider attestation in place of Hepatitis C Commitment Form
- Refills by patients with documented substance abuse will be reviewed by pharmacy on a routine basis
COVID Vaccine & Treatment Overview
COVID-19 vaccines and Health Alliance coverage
- Clinical research is ongoing and information is constantly changing, so please check CDC, IDFA, and American Society of Health System Pharmacists websites to stay up-to-date
- Note: Emergence of new virus variants during Johnson & Johnson phase 3 vaccine trial complicates questions about its efficacy vs. mRNA vaccines; it’s an apples and oranges comparison
- HA coverage
- Medicare: admin fee covered under original Medicare FFS (vaccines covered under EUA)
COVID-19 treatment options and Health Alliance coverage
- Note: Patients who have been given any antibody or plasma treatment for COVID-19 must wait 90 days before receiving an mRNA vaccine
- HA coverage
- Bamlanivimab, casirivimab/imdevimab, baricitinib (Olumiant®)
- Medicare: admin fee covered under original Medicare FFS (drug covered under EUA)
- Rendesivir (Veklury®)
- Medicare: covered under Part B
- Bamlanivimab, casirivimab/imdevimab, baricitinib (Olumiant®)
Convalescent plasma: covered under EUA