URGENT FLASH: Checking Prior Authorization Requirements in Tapestry Link
March 21, 2024Health AllianceTM recently updated the Prior Authorization Routing tool available within the Tapestry Link. With the update, it’s now possible for you to check the prior authorization (PA) requirements for a specific patient (who’s a member of one of our plans), based on their specific plan, coverage and benefits.
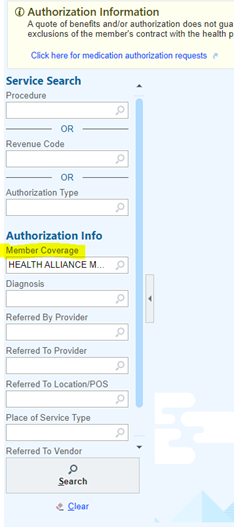
After you log in to the portal, you’ll choose the “Select Member” tile on the home screen. After you’ve entered your Health Alliance member information and are attached to the member, you will choose the “New Authorization” or “Prior Auth Routing” tab. When attached to a member, this screen will populate certain fields and will allow you to begin your search for CPT or HCPCS codes.
Please note that a new field titled “Member Coverage” is required for each search. The Member Coverage field will populate by default.
- We recommend checking the Member Coverage and ensuring the field populates each time you perform a search. If you clear the search, you’ll need to choose the Member Coverage again.
- When accidentally left blank, the Member Coverage field assumes that there’s no Member Coverage or eligibility, and the search will return a result indicating that the service is not a covered benefit.
For your reference, the Health Alliance Tapestry Link User Guide is available under the Digital Tools and Guides on the Provider Resources site.
Please contact our Customer Solutions team or your Provider Relations Specialist with any questions.